The Claim Submission Report can be used to view claims submitted to insurance within a selected date range, grouped by desired categories such as submission date, submission user, financial class, provider, or service location. The report includes a summary tab with a summary of the current month's numbers that include; Claims Submitted, Distinct Claims Submitted, and Submission Success Rate. It will also provide an advanced search option with the capability of claim drill-down allowing the billing team to quickly review the claims that have been submitted.
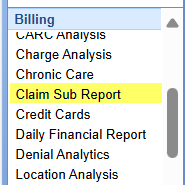
- Open the Reports Portal in the lower left corner.
- On the left-hand side of the navigation pane, choose the Claim Sub Report from the Billing section.
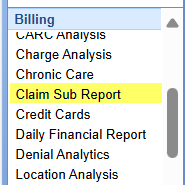

The Claim Submission Report can be found in the Reports portal under the Billing category on the navigation bar. This report by default will open with this month's total in the Submission Summary tab.
The date parameter on the Submission Summary tab can can be found in the left upper corner. The This Month button will reset the summary back to the current month. The less than and greater than buttons can be utilized to toggle back or forward a month at a time. The calendar icon will open the calendar allowing you to select a month within the calendar view.
There are 3 totals that are displayed in the Submission Summary tab; Claims Submitted, Distinct Claims Submitted, and Submission Success Rate.
- Claims Submitted: this will provide the quantity of claim batches, quantity of claims, and the quantity of rejections that were submitted based on primary, secondary or tertiary payer submission.
- Distinct Claims Submitted: this will provide the unique claim quantity, total charges and balance that were submitted based on primary, secondary or tertiary payer submission.
- Submission Success Rate: this will provide the quantity and percentage of claims that had a single submission to a given payer.

The Claim Submission Report can be found in the Reports portal under the Billing category on the navigation bar. The Advanced Search tab of this report can be found on the right upper corner of the report. The Advanced Search tab allows a user to enter specific search criteria to run the Claim Submission Report by.
Advanced search fields
- Date Type: The date type that will be utilized to run the report. There are 2 different date types; Claim Submission, or Service Date. The default selection will be Submission Date.
- Group By: This allows the user to select what the grouping on the report will be. The field selected here is what the returned information on the report will be grouped by. The default selection will be Submission Date.
- SubGroup By: This allows the user to select an additional grouping on the report. The default selection will be Submission User.
- Submission Type: This allows the user to filter for primary, secondary, or tertiary submission(s).
- Submission Method: This allows the user to filter for electronic, or paper submission(s).
- Submission Rejections: This allows the user to filter for rejected claims, or non-rejected claims submission(s).
- Submission Users: This allows the user to filter for a user who created the claim submission(s).
After running the report, results will be displayed based on the group by, and subgroup by selection.
To drill into the detail of any grouping click the group row.
After drilling into the Claim Submission Report, you will see the Claim Submission Report with the appropriate detail based on your selection.
The Claim Submission Report contains the following information:

- Claim ID: The ID of the claim. This selection will open the selected claim.
- Created: The date the claim was created.
- Claim Status: The current claim status.
- DOS: The date of service of the claim.
- Claim Charges: The total charge on the claim
- Claim Balance: The total remaining balance on the claim.
- Rejection: The rejection reason on the claim.
- Last Submission: The last date the claim was submitted.
- Submission ID: The claim submission id the claim is displaying for.
- Submission Date: The date of the claim submission the claim is displaying for.
- Submission Type: The payer level the claim was submitted for (primary, secondary, or tertiary).
- Submission Method: The method the claim was submitted (electronic or paper).
- Submission Payer: The payer the claim was submitted to.
- Submission Count: The total number of times the claim has been submitted.
- Patient ID: The patient's account number.
- Patient Name: The full name of the patient, in "[Last Name], [First Name] [Middle Name]" format.
- Primary Count: The number of times the claim has been submitted to the primary payer.
- Primary Payer: The primary payer on the claim.
- Secondary Count: The number of times the claim has been submitted to the secondary payer.
- Secondary Payer: The secondary payer on the claim.
- Tertiary Count: The number of times the claim has been submitted to the tertiary payer.
- Tertiary Payer: The tertiary payer on the claim.