New Features and Updates
General
Comments and Alerts
- U14546 - Patient Comments and Claim Comments: The Comments and Alerts window was previously updated however the new screen had not been available in all areas. In this release all windows have now been updated to display the newer Comments and Alerts window. More information may be found here.
iScheduler
Appointment
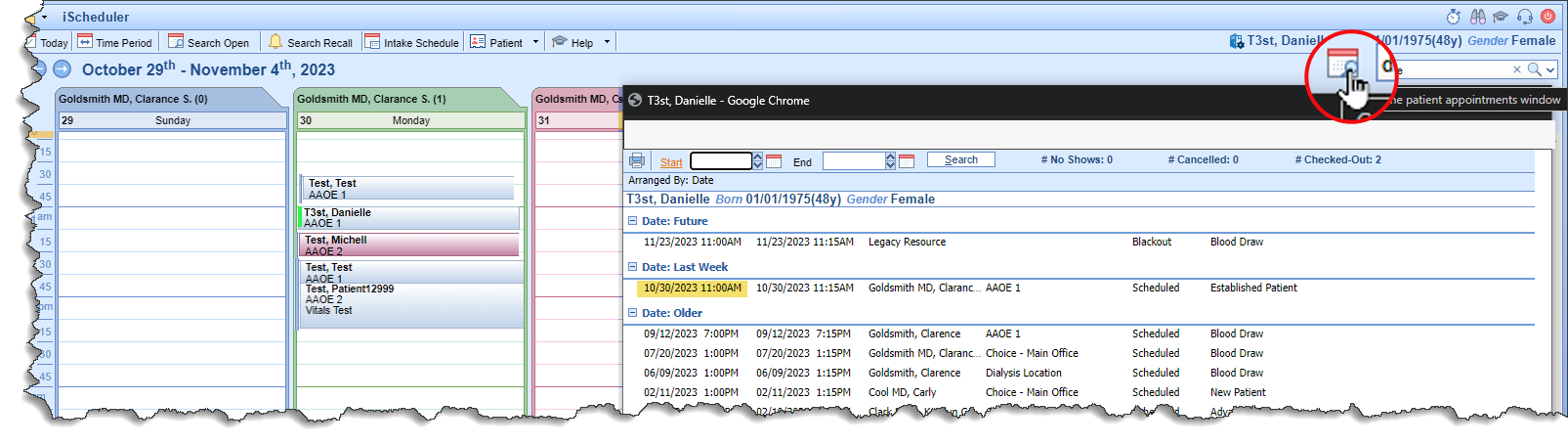
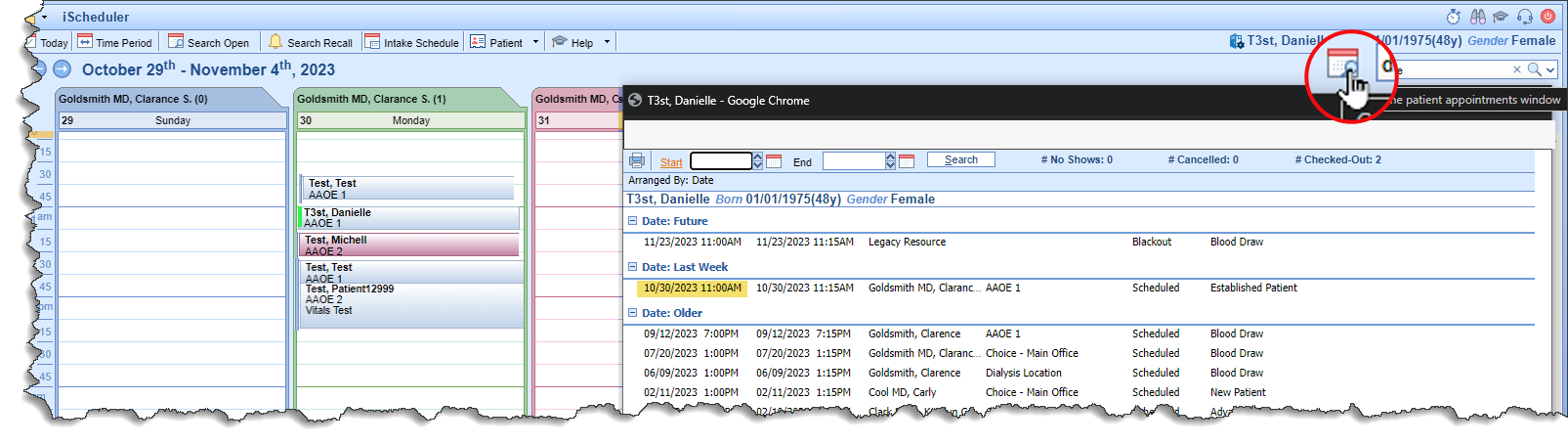
- U15552 - Appointment History Shortcut: As part of our initiative to improve front office workflows, an Appointment shortcut has been added on the iScheduler screen. When the patient is searched, select the calendar icon to the left of the search tool and the appointment list for that patient will display. If a patient is checking in but doesn't recall the specifics as to the Provider or time of the appointment this will make it easier to find that information.
Billing
Claim Query
- U16452 - Recent Patients List: This feature has been active in other areas and is now available within the Billing module. This will allow both access to the Recent Patients list in the Billing module as well as adding to the Recent Patients list in other areas. More information may be found here.
Payment Posting
- U10343 - Credit Balance Access: The Credit Balance feature may be accessed several ways for processing individual claims including Patient Setup, Patient Transaction History as well as Claim Query. More detailed information may be found here.
- U16628 - Credit Balance Adjustment Comments: A double asterisk (**) will be in front of the dollar amount for the Adjustment Comment. This is a visual indicator that the adjustment amount is not being added to the adjustments total and is an adjustment comment.

Bug Fixes
General
Authorization
- B15172 - Duplicate Authorizations when double clicking: Corrected the action of double clicking "Ok" or "Apply" when creating an Authorization so that it no longer duplicates the authorization entry.
MIPS Dashboard
- B16597 - MIPS Provide Patient Access Measure Logic Update: The MIPS 2023 Provide Patient Access measure numerator logic has been updated to support "incident to" billing scenarios where a patient is seen by and has an appointment with a mid-level clinician and the visit is billed under an MD/another clinician. We have updated the measure numerator to take into account the FHIR Received CCDA's NPI or Appointment ID to account for these "incident to" encounters. This was hot fixed post release for Release 23.18.
- B16600 - MIPS Dashboard Patient Measure Count Timeout Error: For our larger practices, users were getting a 500 error when trying to pull the Patient Counts at the Group level for MIPS Promoting Interoperability measures. The Patient Counts are now calculated and stored with the numerator/denominator calculations in the background as a request so users will no longer encounter this timeout error when pulling patient counts for the MIPS Group Measures. This was hot fixed post release for Release 23.18.
Billing
Claim Submission
- B16464 - Auto Submit Batches: When the auto submission process batches claims overnight, some batches were too large causing issues when trying to view them later. This has been corrected to create smaller batches to load more quickly when viewing details later.
Credit Balance
- B16620 - Credit Balance Transfer Omitting Cents Value: Processing a credit transfer from the Credit Balance window was corrected to display the cents value on the destination claim.
- B16621 - Credit Balance Transfer included Adjustment Comments: On the Payment Transfer window within the Credit Balance screen, the adjustments included Adjustment Comments. This has now been corrected.
- B16638 - Credit Balance Destination Claims Filtering: Credit Destination claims were including insurance balance claims. This has been corrected to only include patient balance claims.
Reporting
- B15066 - Payment Listing Report: Corrected an issue where the Payment Listing By... reports under Practice Summary Report weren't calculating payments and adjustments the same as other payment reports.