Executive Summary
Patient Cost Estimator | Split PDF |
Batch Payment Posting | CKCC |
New Features and Updates
General
Patient Cost Estimator
- E13508 - New Patient Cost Estimator Tool: Created a new tool which will assist practices in giving patients an estimate of charges they will be responsible for prior to receiving services. To learn more about this tool click here.
Split PDF
- E11161 - New option to Split PDF documents: Added a new feature which will allow Practices to split faxed/scanned PDF documents into single pages or group them into related pages. To learn more about this feature click here.
CKCC
- E14163 - New CKCC Case Management module: Implemented a new CKCC (Comprehensive Kidney Care Contracting) case management module that will aid Practices by improving visibility and tracking of CKCC Patients. To learn more about this feature click here.
Webservices
- U14388 - Updated Webservices for Patient Demographics: In order to account for RHC date changes in Patient Demographics, the Webservices have now been updated.
Reports
Connect
- U14828 - New 'Charges by Appt Type' report: Created a new Connect report called Charges by Appointment Type which returns a listing of charges based on appointment type/date range. To learn more about this report click here.
- U14826 - New CCM Patient List report: Created a new Connect report called cc_datav1 which returns CCM Patients with Medicare or Medicare Replacement Class Insurance. To learn more about this report click here.
Billing
Batch Payment Posting
- E9149 - New Batch Payment Reconciliation Tool: Added an optional Batch Payment tool which will allow Practices to create, manage, and balance to batches of posted payments (both Insurance and Patient.) To learn more about this new option click here.
Claims
- U12061 - New 'Error Type' search filters: Added additional error filters to the Advanced Search of the Ready to Send screen (users will need to check these new columns in the More > Display Settings menu in order to see the new columns.) These new filters include:
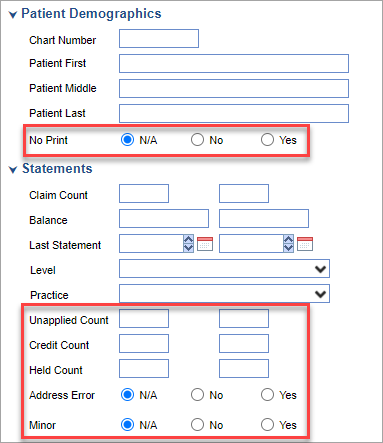
- Patient Demographics
- No Print
- Practice
- Unapplied Count
- Credit Count
- Held Count
- Address Error
- Minor
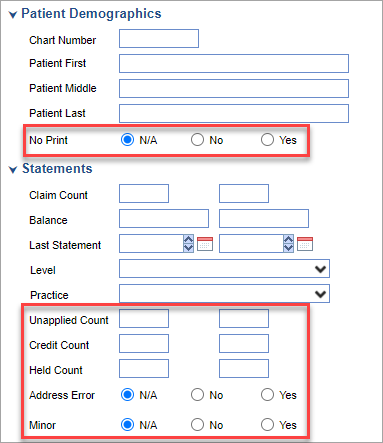
- Patient Demographics
Statements
- U13817 - Added Patient Name Suffix to Statements: Patient Name suffixes such as Jr., Sr., etc will now display on Statements.
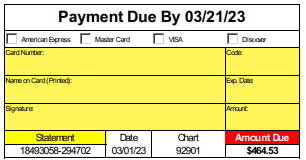
- U13275 - Increased field sizes on Payment Due box: In order to allow more space for Patients to fill out payment information on Statements, Practices now have the ability to increase the size of those fields:
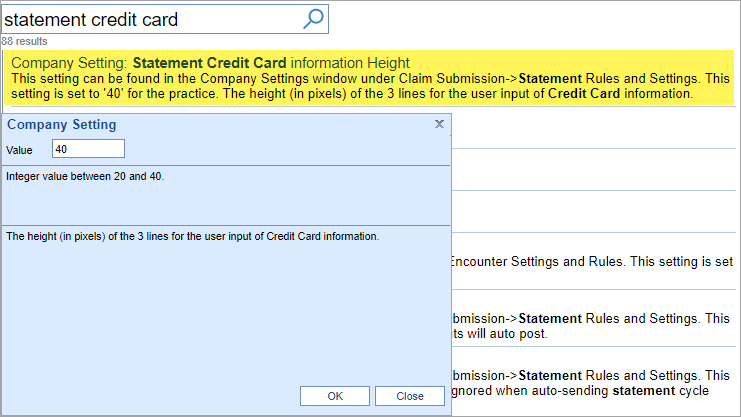
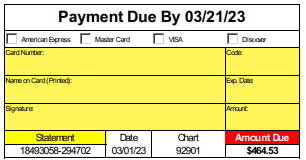 These field sizes can be controlled by a Company Setting called Statement Credit Card Information Height:
These field sizes can be controlled by a Company Setting called Statement Credit Card Information Height: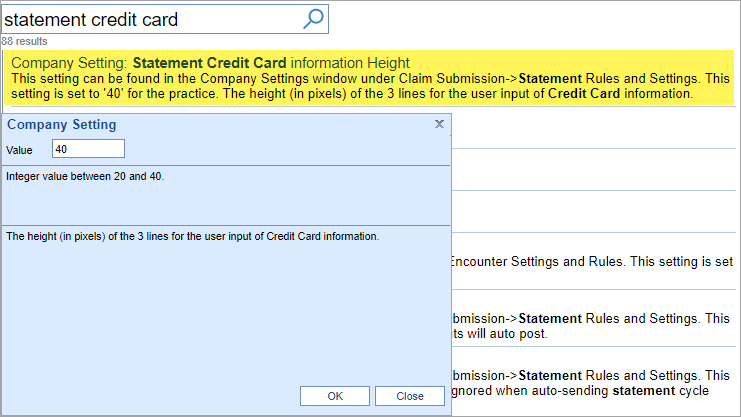
Bug Fixes
General
Comment Editor
- B14731 - Pasting text overwrites existing comments: In the new Comment Editor, if text was pasted in using the CTRL+V keyboard shortcut, it was overwriting existing comments instead of appending to them.
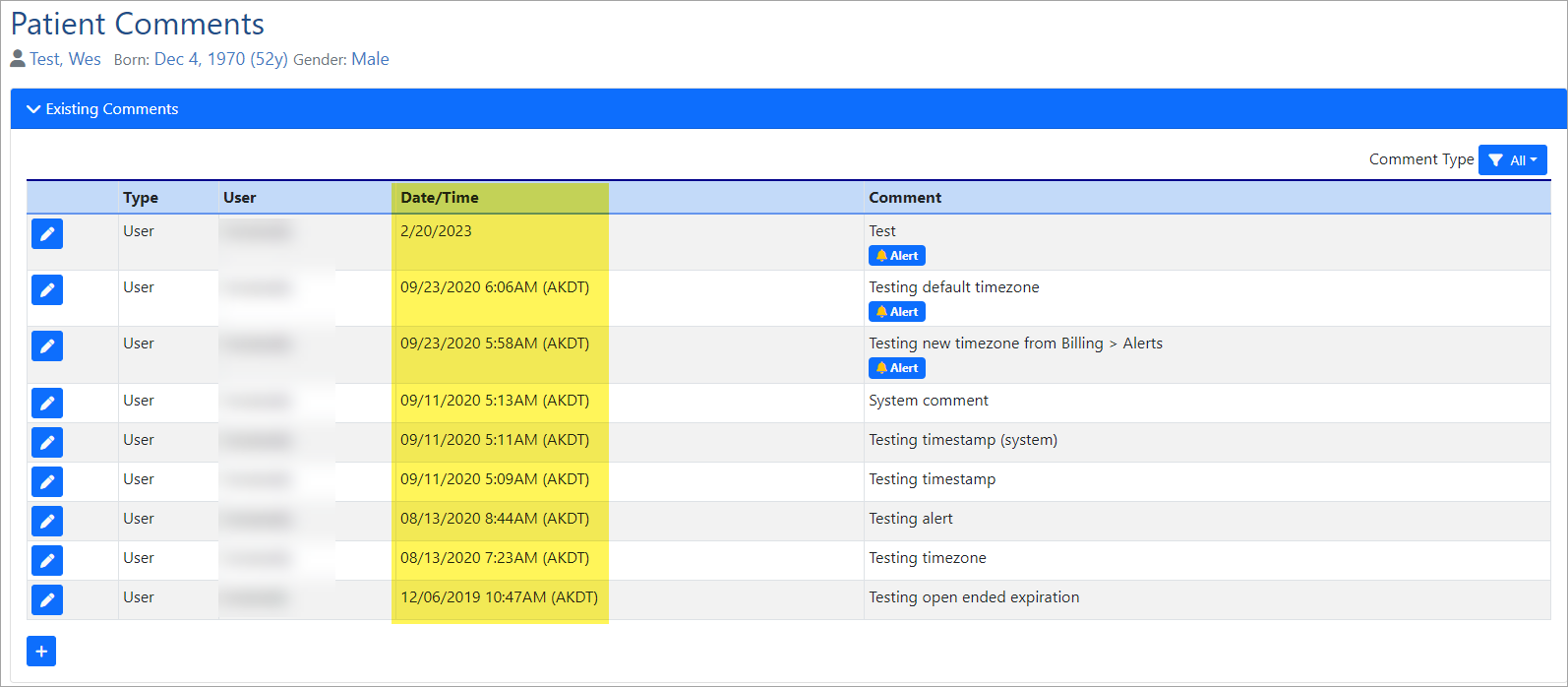
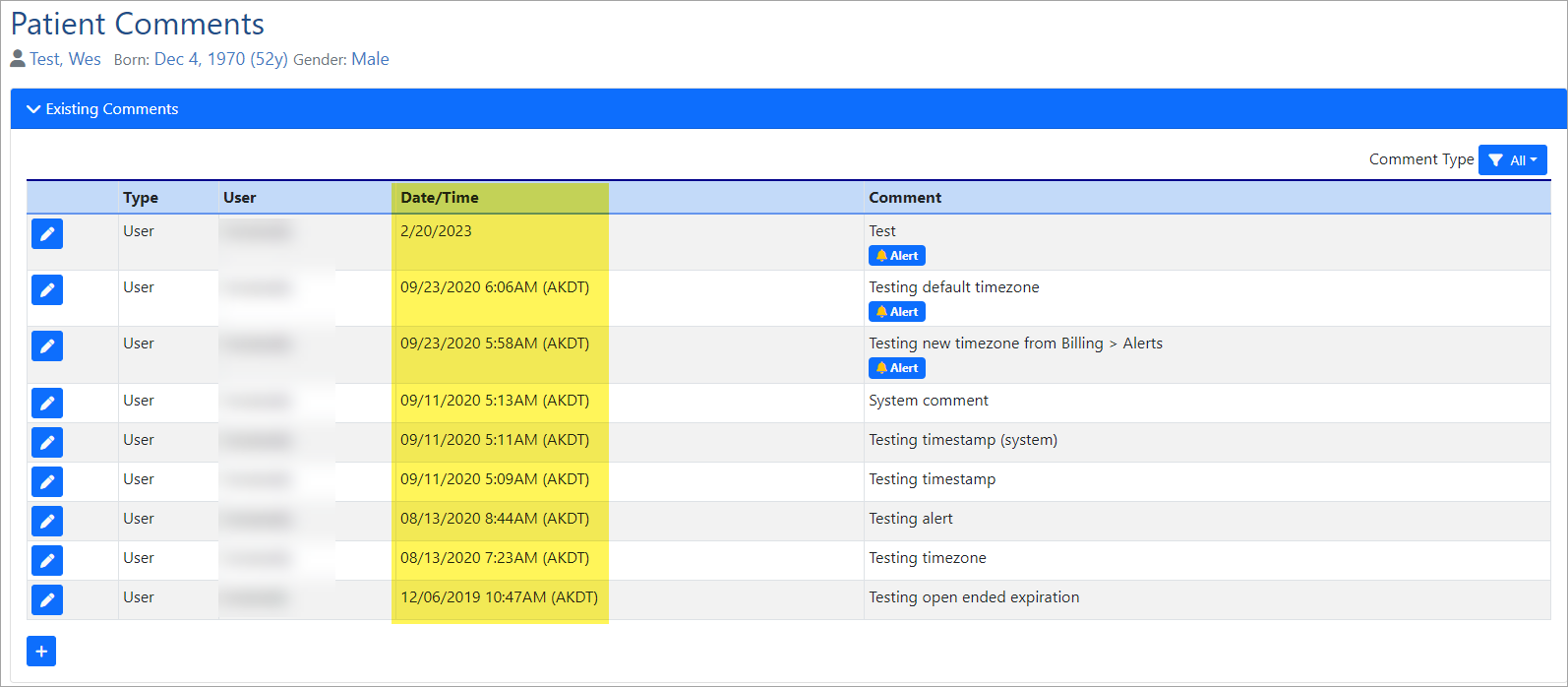
- B14718 - Comments not ordered correctly: The new Comment Editor window was displaying the Date/Time column from oldest to newest, instead of displaying the most current comments first:
Billing
Claims
- B14713 - Pre-existing Appointments not populating Insurance Profile on Claims: The new Insurance Profile logic was implemented in Release 23.02. However, for appointments that were created prior to Release 23.02 where the Superbill was created from the Quick Pay window, the new Insurance Profiles were not carrying over into the Claim.
Reports
- B14562 - Practice Summary Report update: When filtered on Deposit or Deposit Post date, the Practice Summary report should return all Payments and Adjustments that where made within the specified date range. However, the report was only returning the Payer and Financial Class payments/adjustments of the Primary payer instead of also including the Payer and Financial Class from whom the payments/adjustments were made.