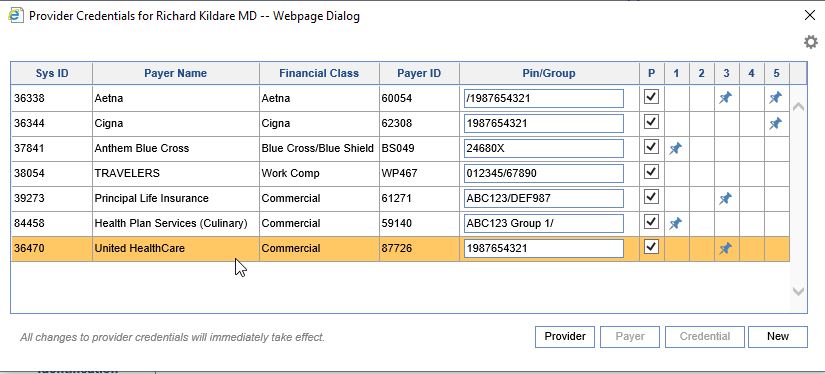
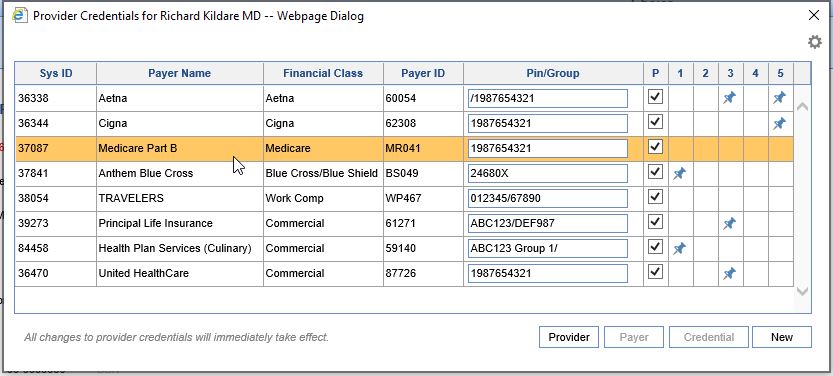
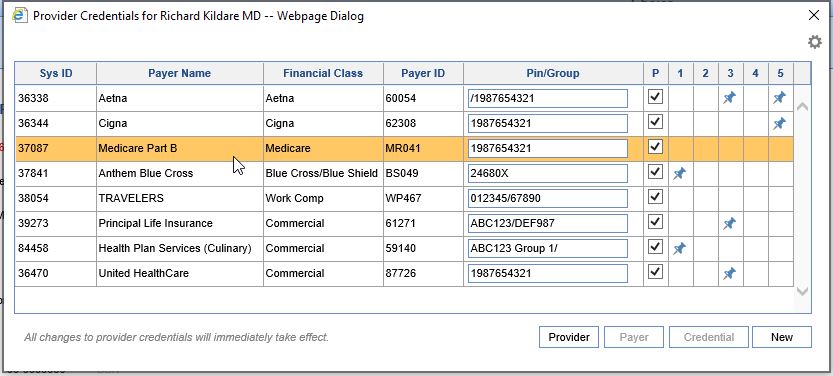
Here are some example situations which might require a Provider Credential:
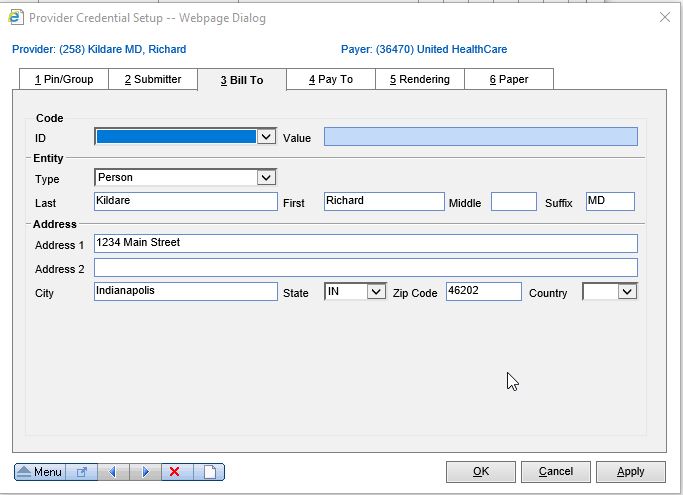
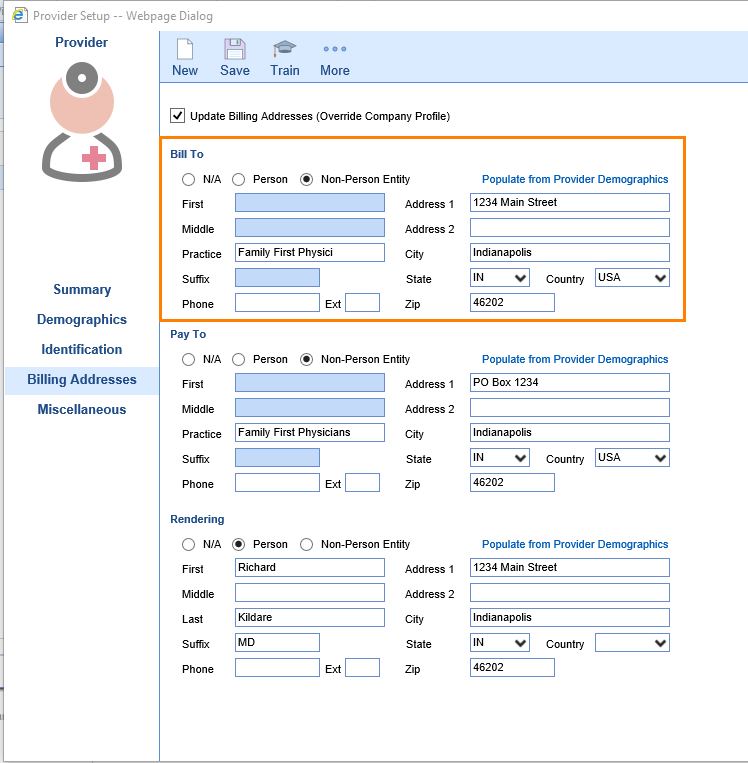
Billing Provider needs to be Individual, not Group:
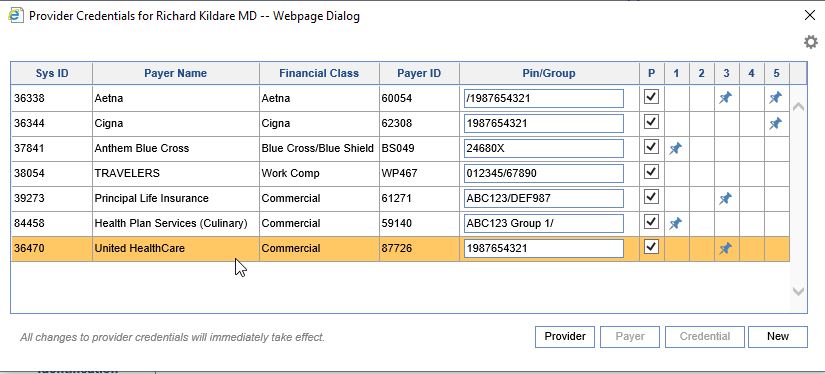
- Create a credential for the affected payer and double click.
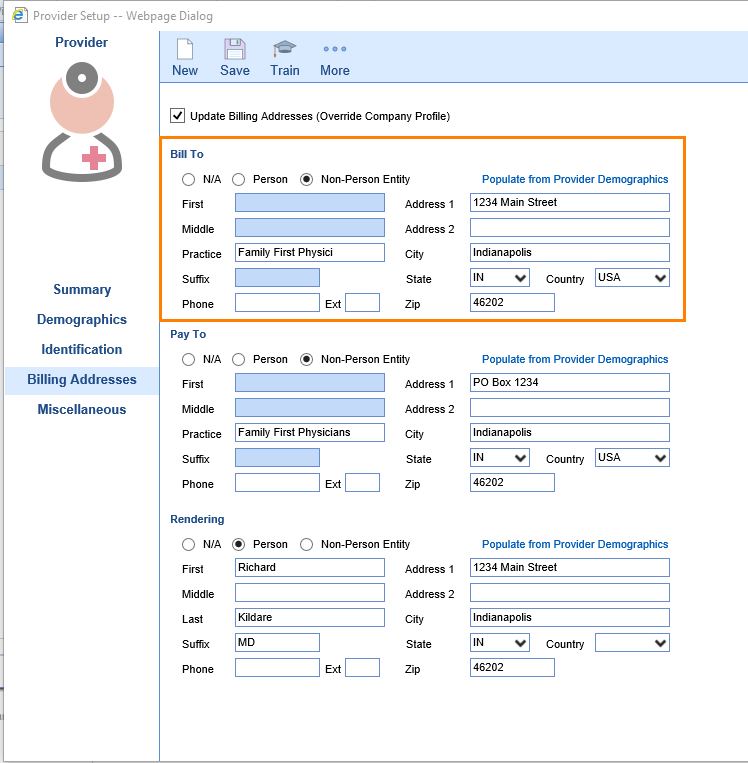
- Go to tab 3_Bill To. Change the Entity Type to "Person" and complete the rest of the information. Save.
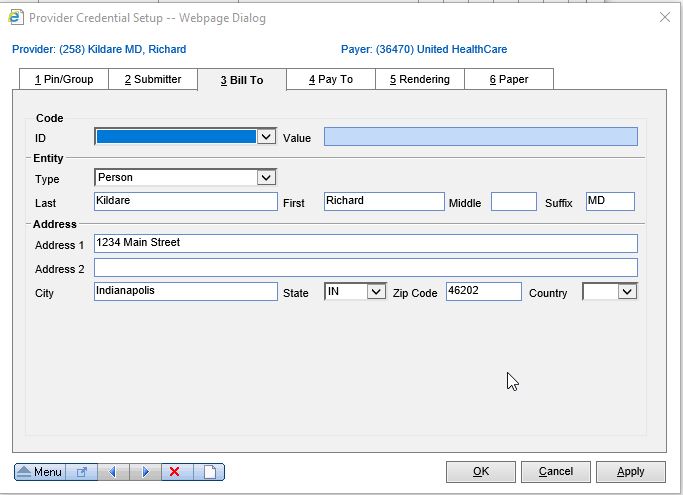
- On claims for this particular payer, the information in the credential will now override the the default information on the Billing Addresses tab.
Add a unique Submitter ID for Medicare (only applies in certain states):
- Create a credential for the affected payer and double click.
- Go to tab 2_Submitter. Enter the Submitter ID as provided by Medicare. Mark the Entity Type as either Person or Non-Person, and enter the Name of the Entity. Save.

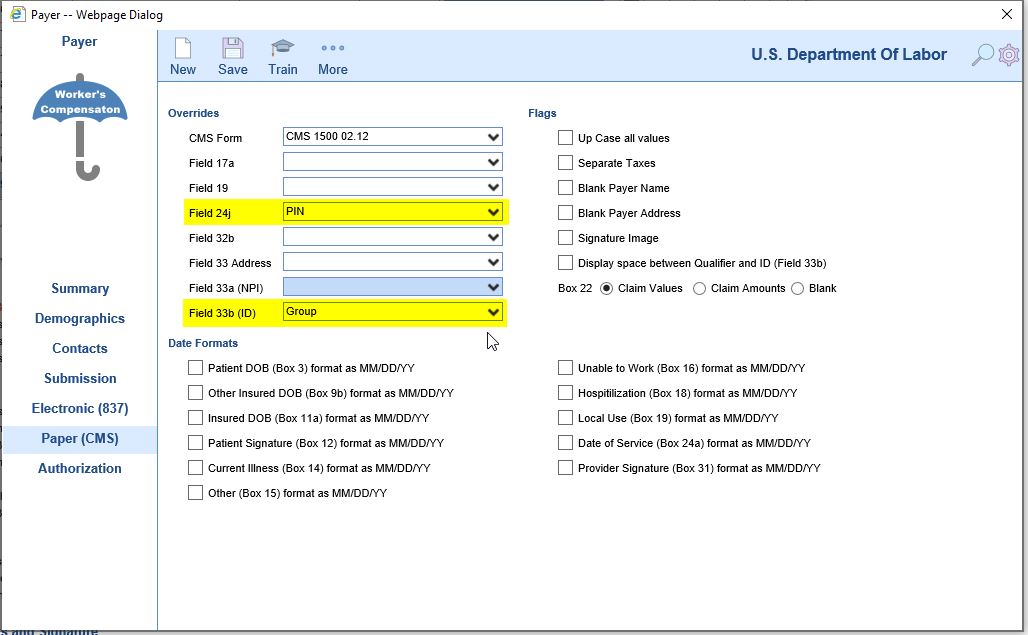
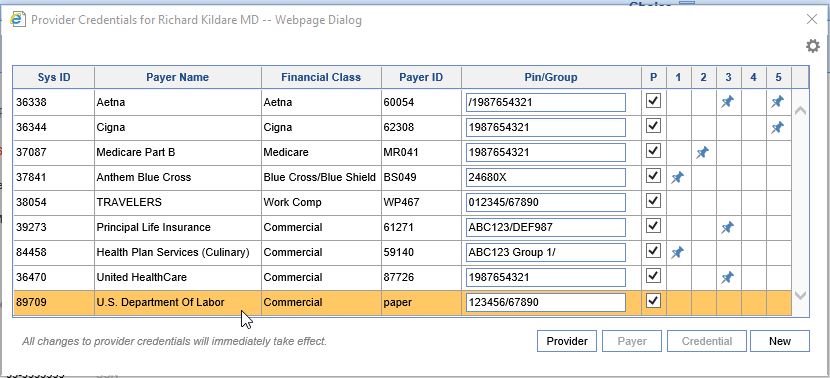
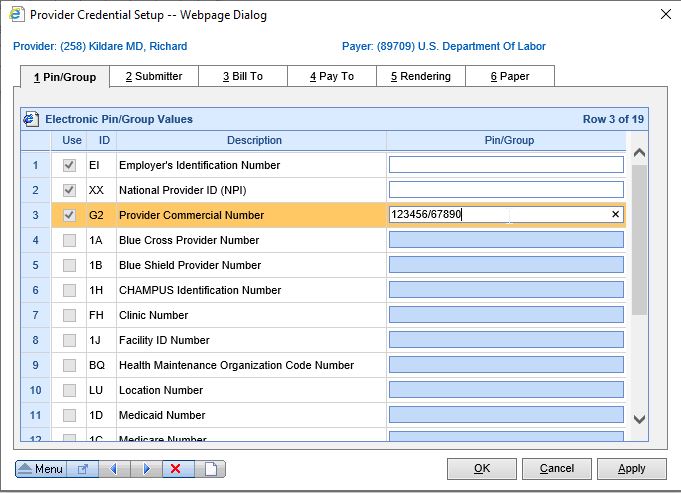
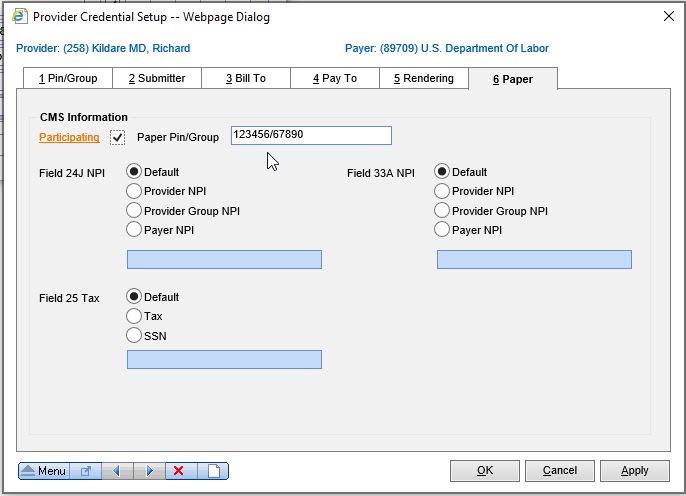
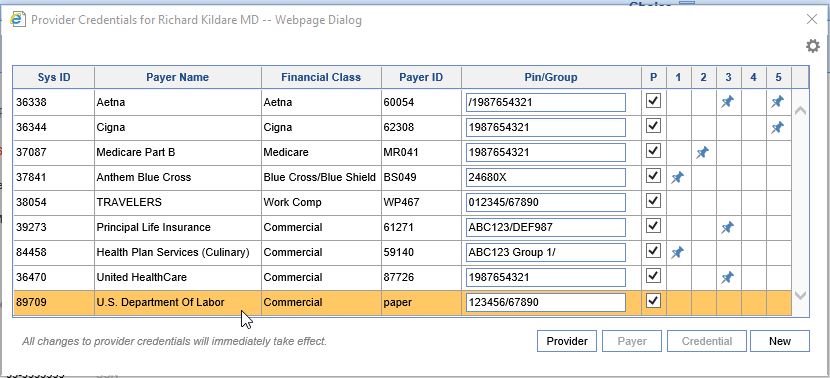
Payer Specific Number needs to be sent on Paper claims
- Create a credential for the affected payer and double click.
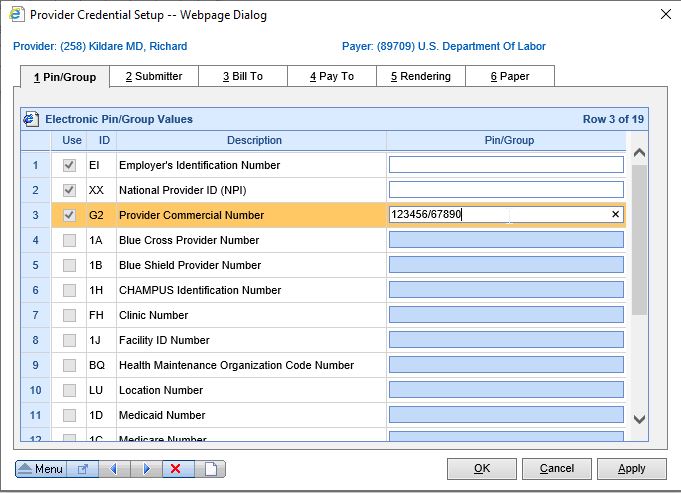
- Go to tab 1_Pin/Group and enter the information in the appropriate field (usually "G2-Provider Commercial Number"). The PIN is usually the providers individual Provider Number, and Group is usually the practice's Provider Number. Anything prior to / is considered the PIN, anything after is the Group.
- Go to tab 6_Paper. The number(s) in the Paper Pin/Group field will be the same as what you entered when creating the credential. If not, or if you did not enter anything when creating the credential, enter the correct Pin/Group information into the field. Save.
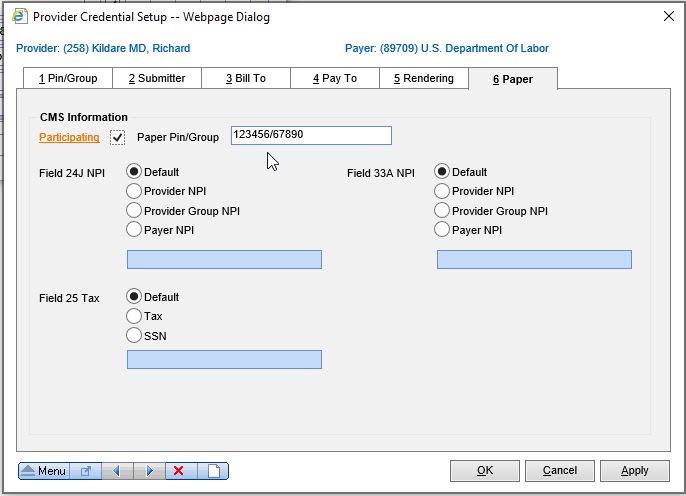
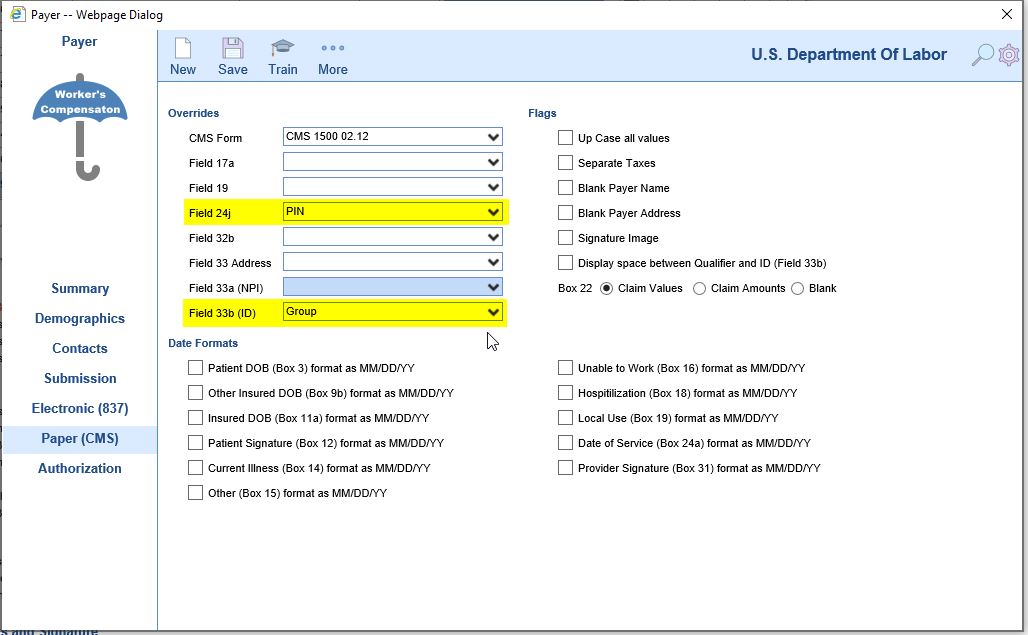
- For these numbers to appear on a claim, the Payer Setup will need to be updated on the Paper (CMS) tab, and selected by dropdown for the appropriate boxes on the CMS-1500 form. Adding the credential is not enough by itself.