Our application has the ability to retrieve prescription cost information based on a patient/drug/pharmacy combination via the CoverMyMeds Real Time Benefit Check integration (RxBC). Once this feature has been setup for your practice, the following options become available:
Benefit Check Process
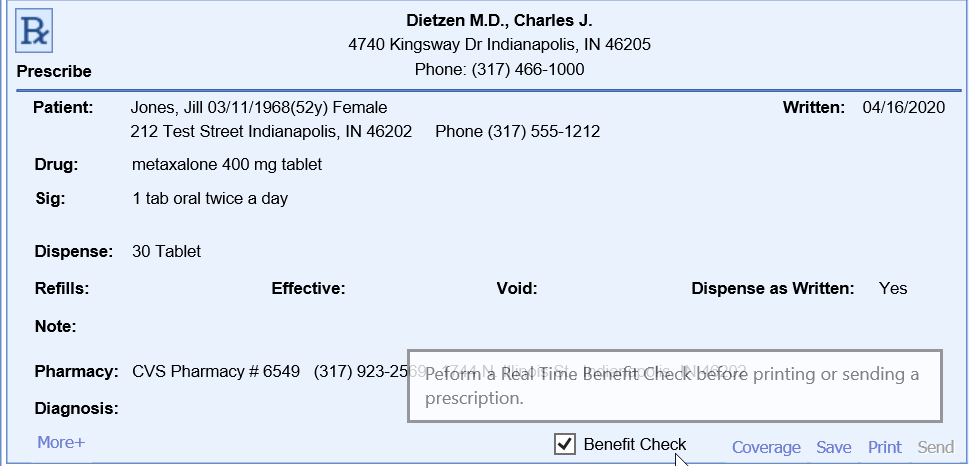
- Navigate to the EMR
- Open a patient chart
- Open the medications chart tab
- Fill out the prescription and select the desired pharmacy
- If you would like for a benefit check to occur, be sure the Benefit Check option is selected. If the product has been activated for your practice, this will be selected by default. Users can override this option by updating their user settings.
- If you would like for a benefit check to occur, be sure the Benefit Check option is selected. If the product has been activated for your practice, this will be selected by default. Users can override this option by updating their user settings.
- Click Send
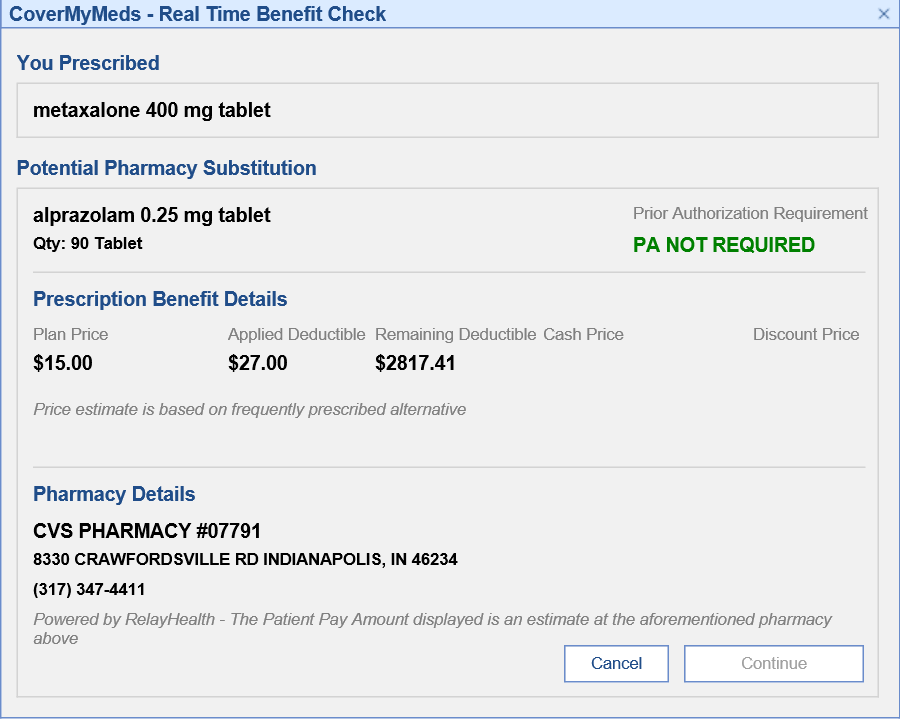
- Before the prescription is actually sent, a benefit check will be displayed providing details on the expected cost.
- If you would like to continue sending the prescription, click Continue. Otherwise, click Cancel to make any necessary changes and restart the process.
Benefit Check Details
| Field | Description |
|---|---|
| Potential Pharmacy Substitution | This provides the drug most commonly dispensed at the pharmacy. This is a true representation of what the patient would experience at the pharmacy. For example, a brand medication is selected during prescribing but the Benefit Check may indicate that the pharmacy selected when receiving this brand medication would typically dispense a generic medication. This would provide the payment and coverage details for the generic medication. If ‘Dispense as Written’ is selected during prescribing, drug substitution will not occur. |
| Prior Authorization Check | Indicates if a Prior Authorization will be required by the pharmacy. |
| Plan Price | A single co pay amount will be returned when the plan/PBM is able to respond with an exact price In the event a single patient pay amount value is unable to be returned, historical pharmacy data is used to return a price range reflective of when the patient’s insurance is used. |
| Applied Deductible/ Remaining Deductible | The response has the ability to provide details around how much of the copay amount applies toward the deductible and what would be remaining of the patient’s deductible. |
| Cash Price | A price range reflective of what a patient would pay when not using their insurance. |
| Discount Price | The discount price field represents the price a patient would pay if they present the associated discount card to the pharmacy. A link will be provided that you must click to print off the discount card. |