Question: One of our claims has rejected for "Claim Frequency Code". How do I fix this rejection?
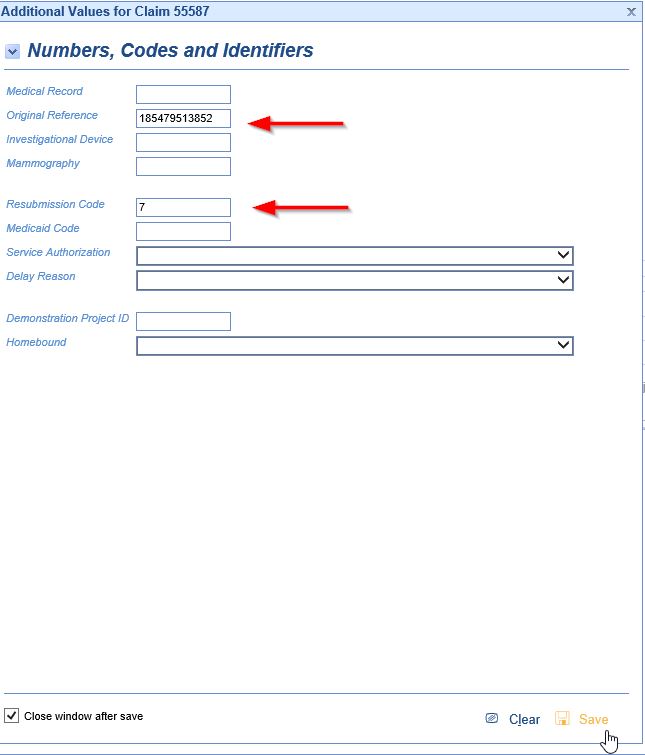
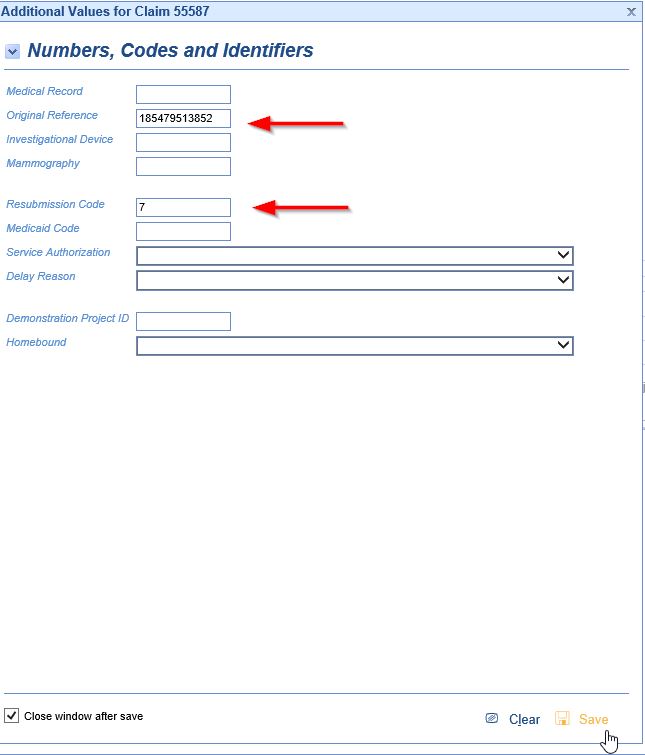
Solution: This particular rejection means that the claim has been sent with a Frequency Code deemed invalid by the Payer. On all claims, the default Frequency Code is 1. For certain payers, when submitting a corrected claim, a 6, 7, or 8 (as appropriate) is entered in the Resubmission Code field in the Additional Claim Information > Numbers, which changes the Frequency Code. Medicare does not accept any Frequency Code but 1. Having something in the Resubmission Code field will cause this rejection.
To fix the rejection, you will need to open the Additional Information > Numbers and remove both the Resubmission Code and the Original Reference Number from the claim.
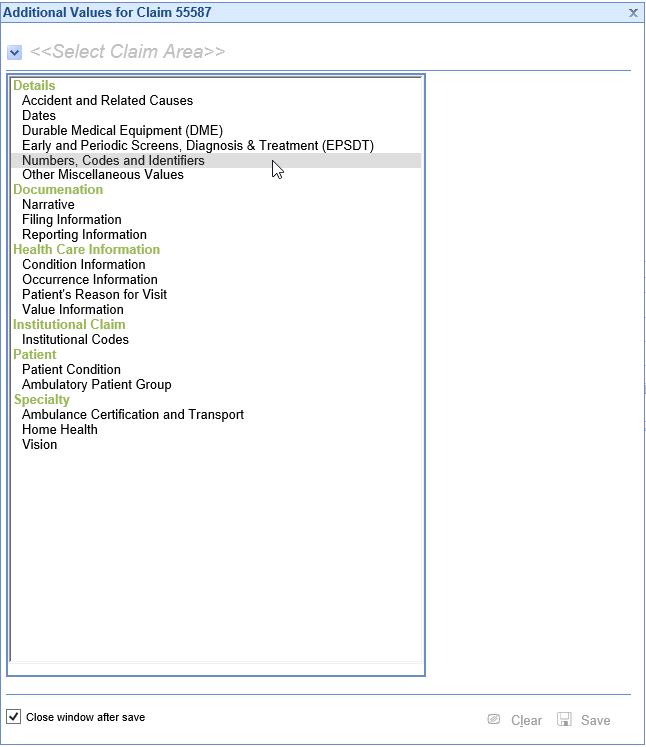
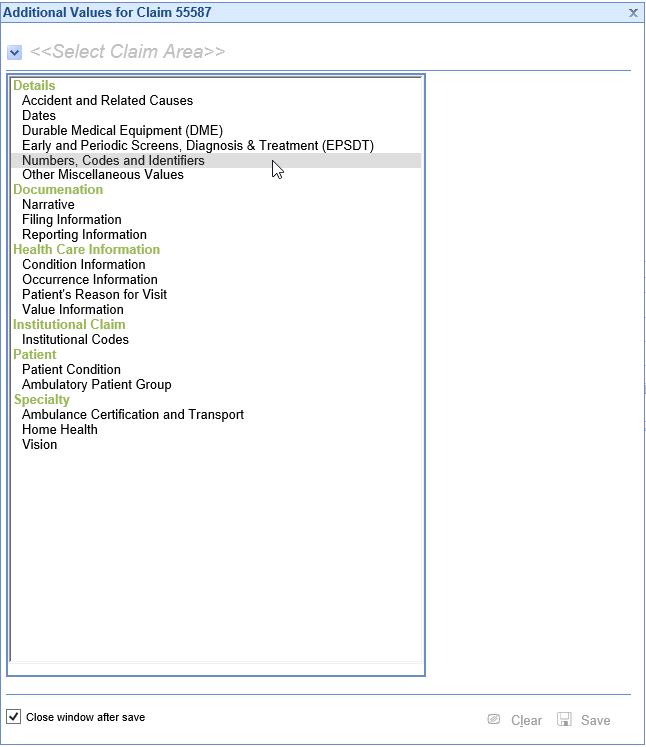
- Open the claim and go to Additional Information > Numbers.
- Delete the Original Reference Number and Resubmission Code. Click Save.
- Before resubmitting the claim, you may need to go add a "Corrected Claim" note in Box 19.