New Features and Updates
Setup
- U18271 - New Company Setting to Replace Chart Correction Text With Practice Desired Text: A new company setting "Progress Notes Chart Correction Text" was created in Setup > Administrative Settings > Company Settings to allow practices to change the wording is the string of text that is used for Chart Corrections. The text input by the practice in the "Company Setting: Progress Notes Chart Correction Text" will replace the default value of "Correction" in the Chart Correction string. It will also update the chart 'Correction' button label and the header label for the Add a Chart "Correction" text box.
The default value will be "Correction." You can enter the value of the word(s) that you want to use as a replacement for the word "Correction" (for example, "Amendment").

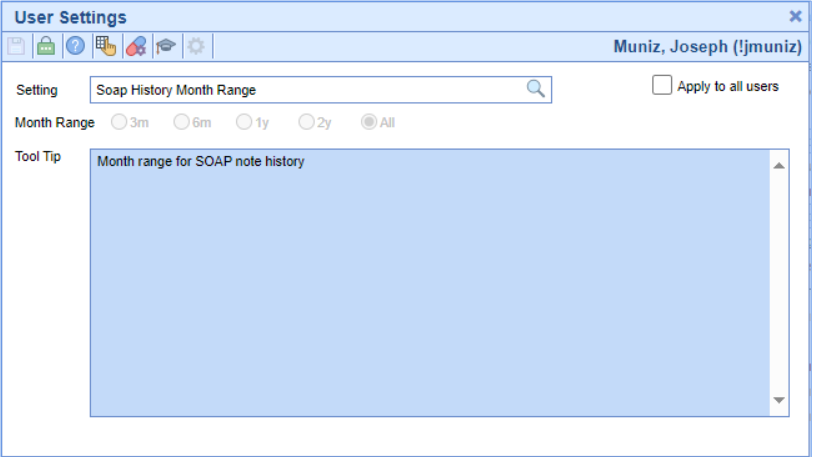
User Settings
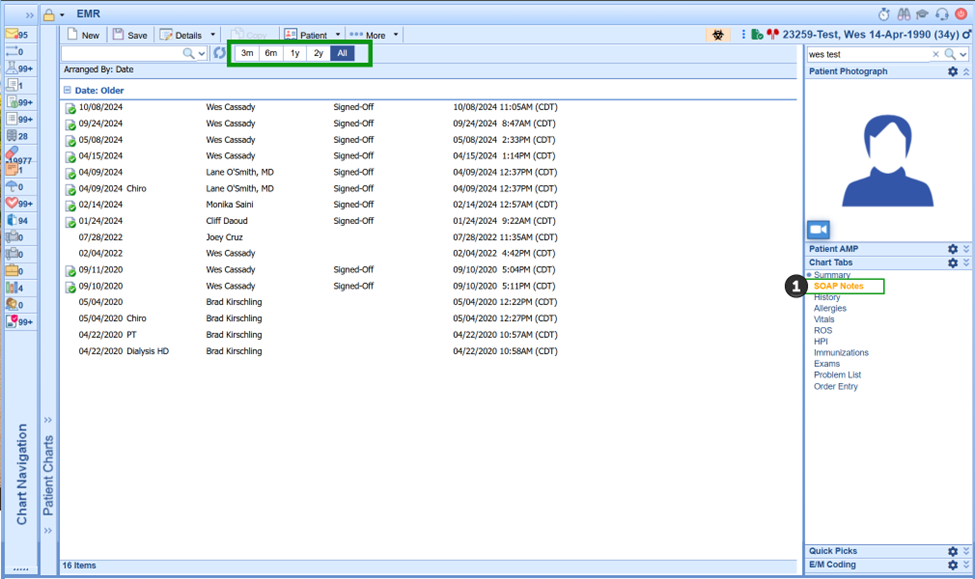
- U18506 - New User Setting For SOAP Note History Performance Improvement: To improve the load time of SOAP Note history for customers with a high volume of SOAP Notes, a new company setting has been created within Setup > Users > User Settings. When set, User Setting: "Soap History Month Range" will allow users to configure how they want their default note history to display. Users will have the option of setting their Soap Note load to pull data for the last 3 months, 6 months, 1 year, 2 years, or All.
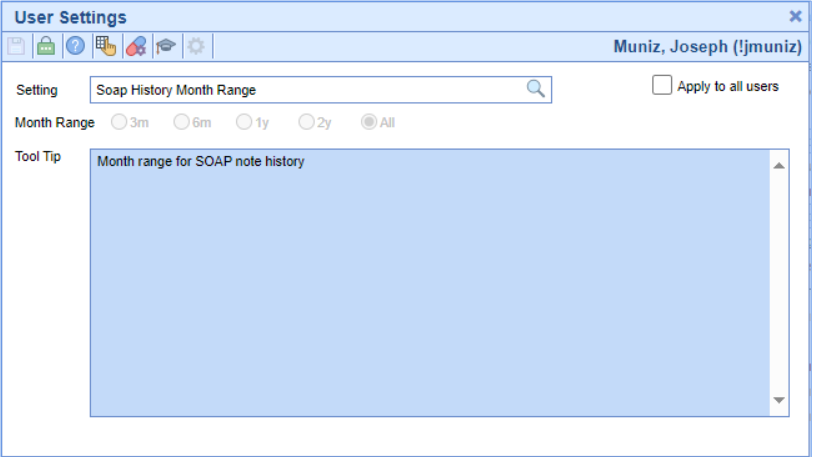 Alternatively, users will see this setting displayed in the SOAP Note history screen (as shown below). Users can update this setting as needed to display their desired look-back period.
Alternatively, users will see this setting displayed in the SOAP Note history screen (as shown below). Users can update this setting as needed to display their desired look-back period.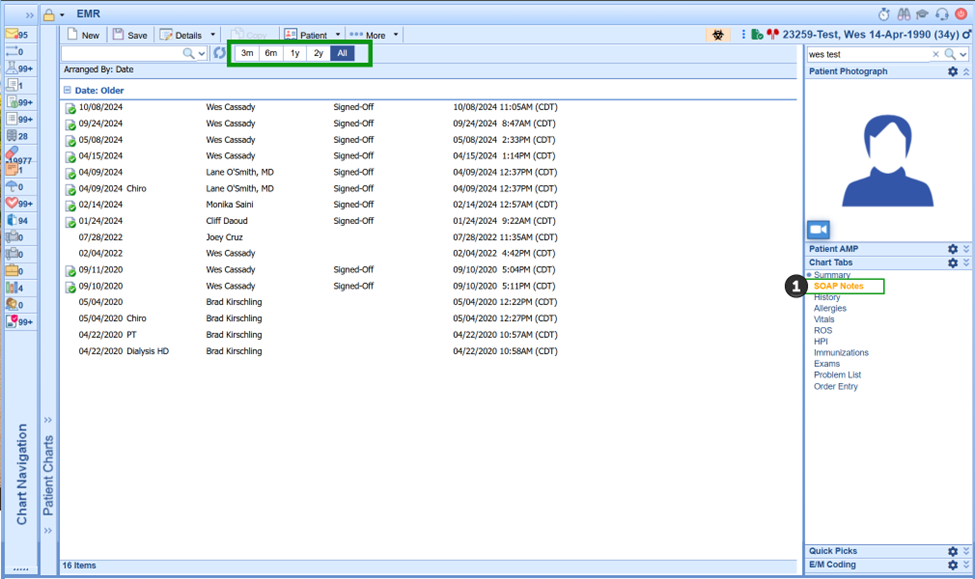
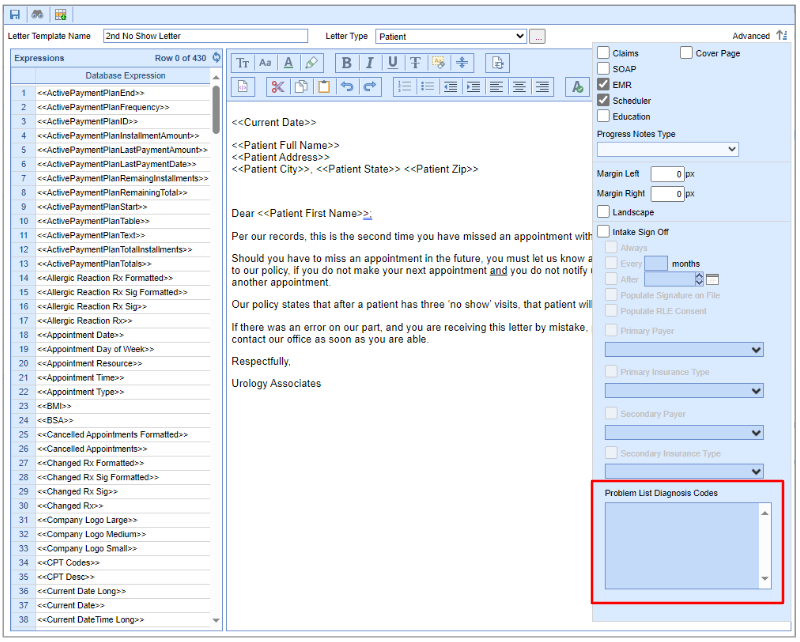
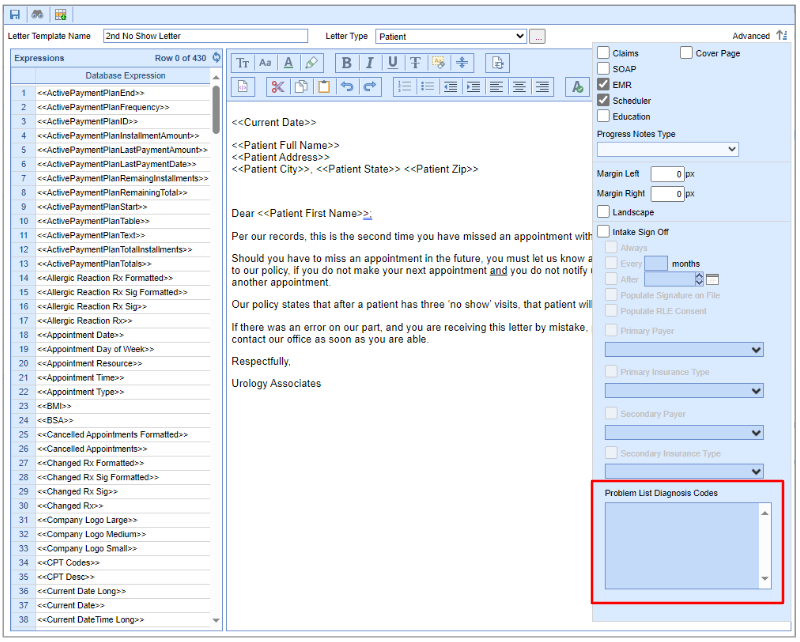
Letters
- U16476 - New Problem List Diagnosis Filter On Intake Letters: Currently, within templates, we have the capability to filter specific sections of an intake or EMR template to be used only when a patient has particular diagnosis codes on their problem list. In this release, we are adding this same functionality to letters. This would allow practices to further customize the data presented to patients, specifically when needing to complete specific consent forms or sign off on patient education forms. Users can configure this filter within Setup > Letters > Advanced > Problem List Diagnosis Codes.
Reports
Connect
- U18350 - Added Patient Email To The Connect Report Claim Status: The Connect Report "Claim Status" is used as a collection report to provide data to collection agencies. While this report included the majority of patient data fields, it did not provide the patient's email address. Since some collection agencies require this data, we have updated this report so that the patient's email field is now included.
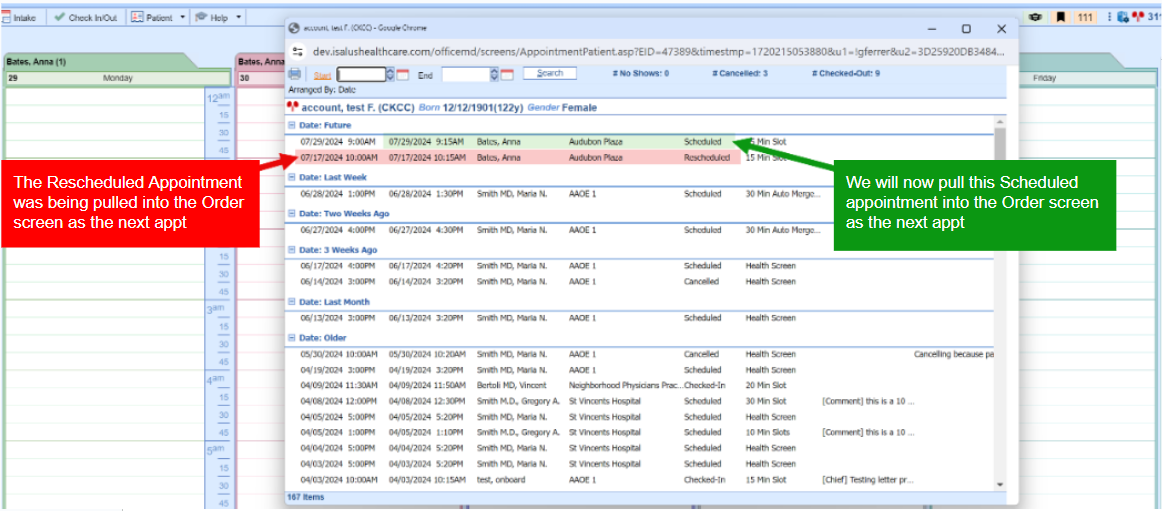
iScheduler
Appointments
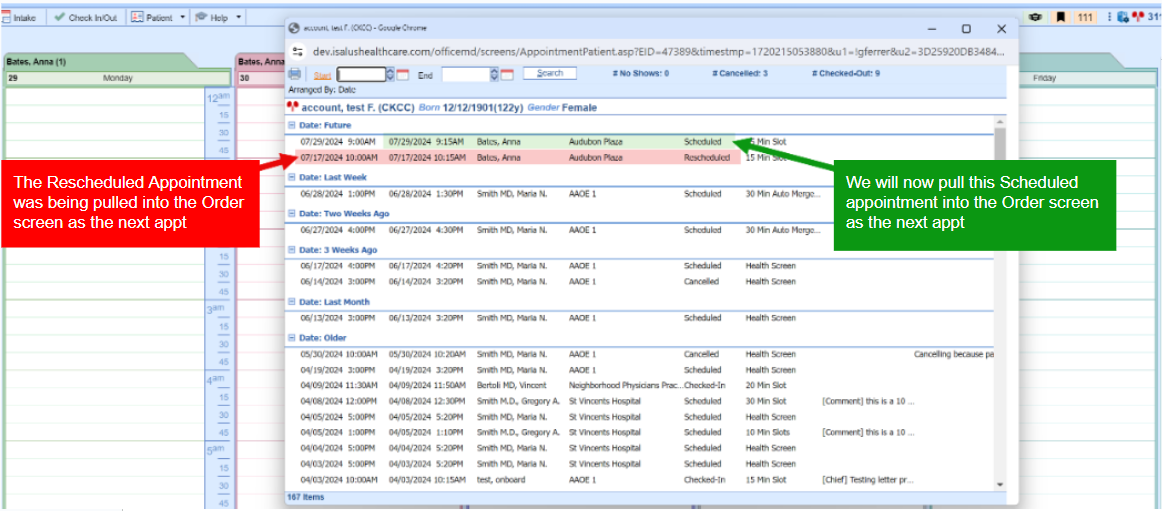
- U18087 - Update Orders not to display Rescheduled Appointments when displaying Next Appointment: When a patient's appointment is marked 'Rescheduled' we were still displaying the appointment as the Next Appointment in the Order screen. To address this issue, we modified the Orders section to exclude appointments with a "Rescheduled" status from being displayed (similar to how we handle appointments with a "Cancelled" status) when showing the Next Appointment.

Bug Fixes
Setup
Company Settings
- B17995 - Company Setting Default Refer. Provider on Patient New Appointment Not Functioning: Resolved an issue in which the company setting "Default Refer. Provider on Patient New Appointment" was not being taken into account when disabled. This caused the referring provider to always be populated in a new appointment when the patient has a referring provider set in their demographics. We have corrected this so that when scheduling/assigning a new appointment and the company setting is set to "No," the referring provider field will not be populated.
EMR Setup
- B18885 - Hospital Rounds | Patients not displaying on the schedule for previous days of a hospital stay if no charges exist and the patient has been discharged: Corrected an issue that could impact practices that use the Hospital Rounds feature. We've fixed a particular situation/scenario in which charges for patients may be missed due to the logic of how the roster is displayed in the EMR. Patients were not being displayed on the schedule for previous days of a hospital stay if no charges existed and the patient had already been discharged. We added an update to allow back charting of hospital rounds for discharged patients under the following 2 conditions:
- The company setting for removing discharged patients from the hospital rounds list is turned off.
- The visit date must be <= discharge date (date the patient was discharged on).
Intake Setup
- B18511- Intakes Not Auto-Merging as Expected: Corrected an issue that was preventing the intelligent intake auto-merge feature from working correctly in specific scenarios. We have modified the code to utilize an update check rather than a read check, which helps better manage this internal error.
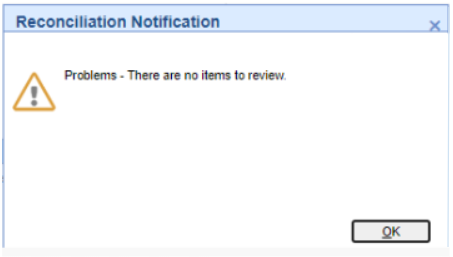
EMR
Patient
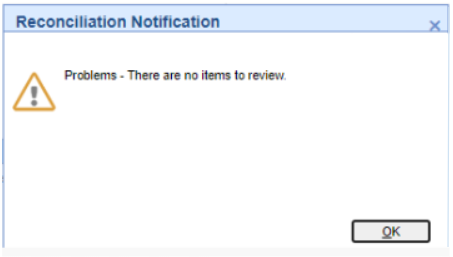
- B18723 - Reconciliation Save Error: "Unable to save review": Corrected an issue that would occur when completing a patient reconciliation process from EMR > Summary (Clipboard Icon) after submitting an Intelligent Intake form, in which a save error would occur if the patient does not have any active problems. The issue was caused by one of the allergies/medications/problems not having any entries. As a result, the message indicated that a review could not be saved because there was nothing to review. We have updated this error message so that users receive a reconciliation notification instead indicating that "There are no items to review."
Billing
Claim Query
- B18629 - Bypass Claim Validation Failing to Save: Corrected an issue that was causing the bypass claim validation to fail to save for a specific claim due to the Diagnosis Code identifier for the procedure being linked to another claim. This occurred because the claim was incorrectly linked to a claim validation on procedure code 99205. The claim validation was bypassed, and the code was overwritten with procedure code 99204. When the new claim was created, the diagnosis code identifier was incorrectly linked to the old claim, and the bypass would not save. We have modified the stored procedure to ensure that the claim and diagnosis are connected so that the bypass works correctly.
Deposits
- B18948 - Deposit Posting Not Updating Claim Status to Done/Completed When Posting Results in $0 Balance For the Claim: Resolved an issue stemming from release 24.121 in which we modified the calculation of how a claim ends up with a credit utilizing a new claim estimated balance. Unfortunately, this calculation was preventing claims that ended up with a $0.00 balance from updating to a Done/Completed status. The issue occurred because the Estimated Balance was incorrectly calculated using Claim Charges instead of the Claim Balance, resulting in the claim status not updating correctly.
- B18962 - Deposit - Claim Missing Payer Error When Remit Status is Secondary: Corrected an issue occurring when a deposit has a claim with a remit status of "Secondary." This was causing the association between the Payer and the ERA payer ID not to happen, resulting in the claim ending up with a missing payer error. We have updated the code to more effectively identify the payer for incoming ERA Deposit Claims.
- B18984 - Deposit Claim Totals Not Reflecting Correct Posting PMT Amount: Resolved an issue that was causing the Deposit Claim Totals to show different Paid amounts between the procedures and Posting PMT. The deposit claim Paid amount was not factored into the Posting PMT amount within the Claim Totals. This issue also caused the balance on the Claim Totals to be reflected incorrectly. We have corrected this by updating the code to get the payments from the Deposit, instead of the payment table.
Payment Posting
- B18845 - Payments and Adjustments Allowed to Be Documented Without Payee: Corrected an instance where a claim balance did not match the Patient Transaction History balance. This occurred because a Payment Transfer adjustment was not tied to a payee. We have resolved this by removing the ability to save a payment with a null/0 payer ID.
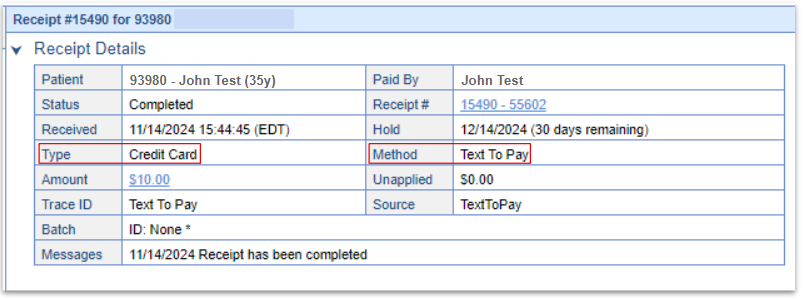
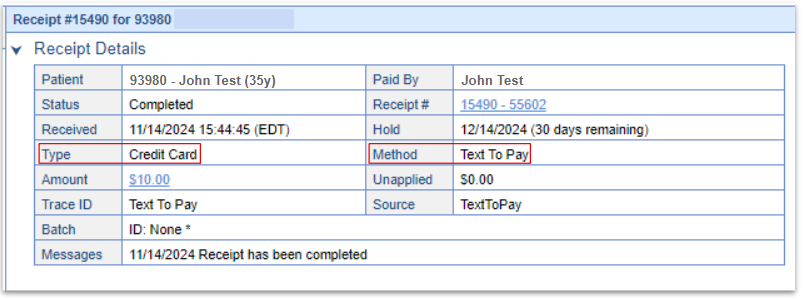
Receipts
- B18944 - Text To Pay Receipt Payment Method and Payment Type Reversed: Corrected an issue that was causing the Payment Type and Payment Method fields of the Text To Pay receipts to be reversed. This means that the Payment Type was being set to Credit Card and the Payment Method was being set to Text to Pay. We have updated this to now set the Payment Type to "Text to Pay" and the Payment Method to "Credit Card."