New Features
Billing
Payments
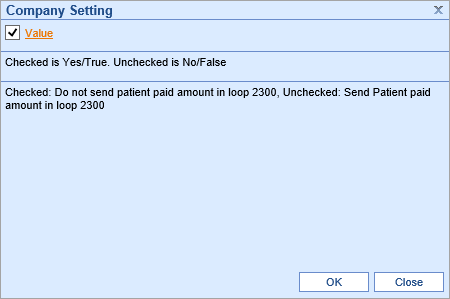
- U11697 - New Patient Paid Amount option: Some Payers have started to process claims differently - including refunding money to patients based on the Patient Paid amount being sent in the 837 files. Because of this, new logic has been implemented that will allow Practices to customize whether they want this information to be included in the 837 files or not. A new Company Setting has been added called, Do not send patient paid amount:
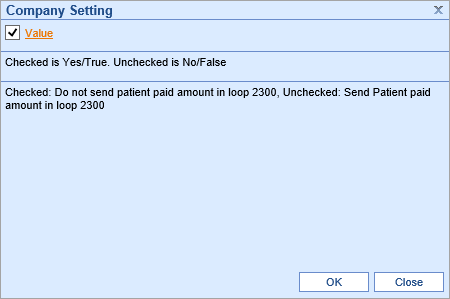 When this setting is checked/enabled, the system will not send patient paid amounts back in the 2300 loop of the 837 files. When the setting is unchecked/disabled, the system will send patient paid amounts back in the 837 files (this is how it worked before.) By default, the setting will be checked meaning this value will not be sent.
When this setting is checked/enabled, the system will not send patient paid amounts back in the 2300 loop of the 837 files. When the setting is unchecked/disabled, the system will send patient paid amounts back in the 837 files (this is how it worked before.) By default, the setting will be checked meaning this value will not be sent.
Updates and Bug Fixes
General
Performance Improvements
- The team has been working hard to identify and optimize various processes throughout the application. With each release, you should see incremental improvements in speed and performance.
Reports
Payment Audit
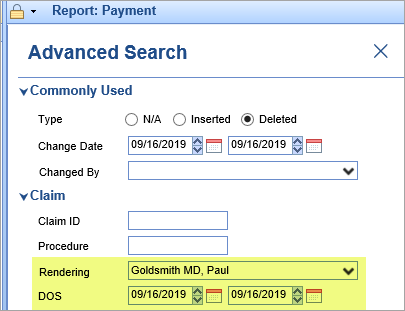
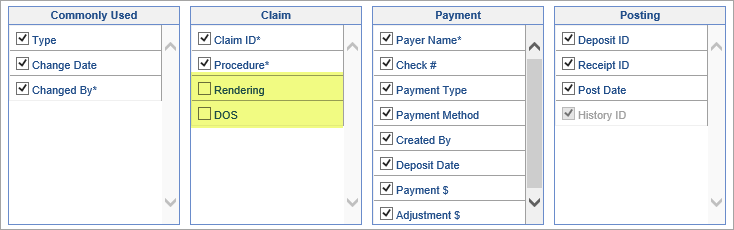
- U11553 - Added Rendering and DOS search fields: Added Rendering (Provider) and DOS fields to the Advanced Search screen of the Payment report:
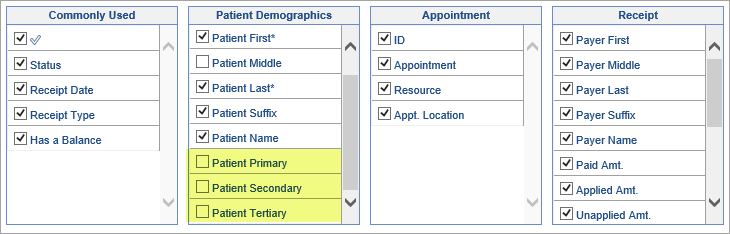
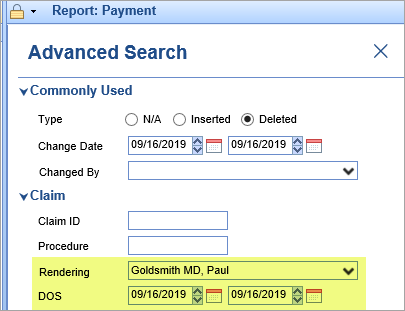 Note: These fields will not display on the report by default. In order to display, they must be enabled in the More > Change Display Settings menu:
Note: These fields will not display on the report by default. In order to display, they must be enabled in the More > Change Display Settings menu: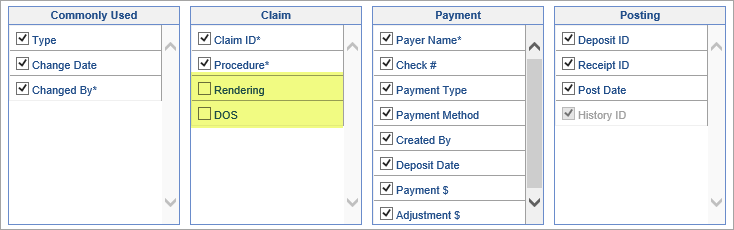
General
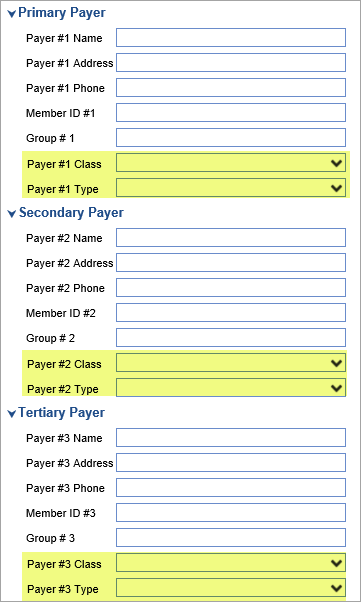
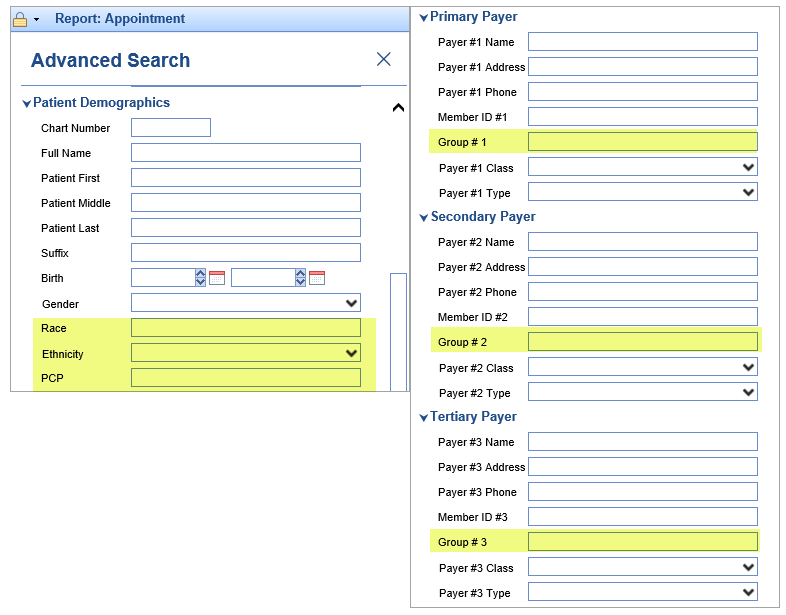
- U8671 - Added additional Demographic and Insurance search fields: Added Ethnicity, Race, PCP (Primary Care Physician), and Group # (Insurance Group/Policy #) fields to the Advanced Search screen of the Appointment report:
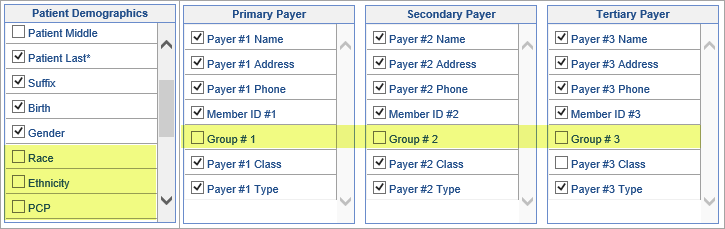
 Note: These fields will not display in the report by default. In order to display, they must be enabled in the More > Change Display Settings menu:
Note: These fields will not display in the report by default. In order to display, they must be enabled in the More > Change Display Settings menu: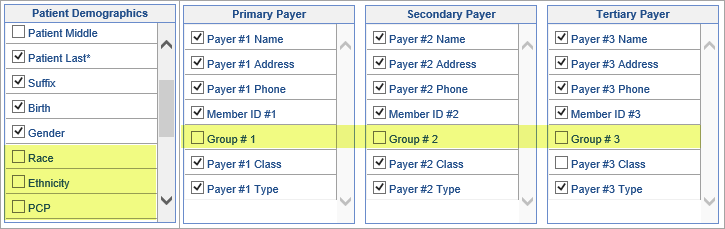
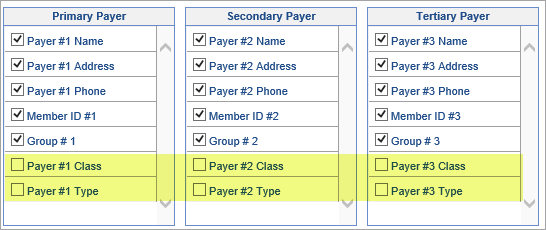
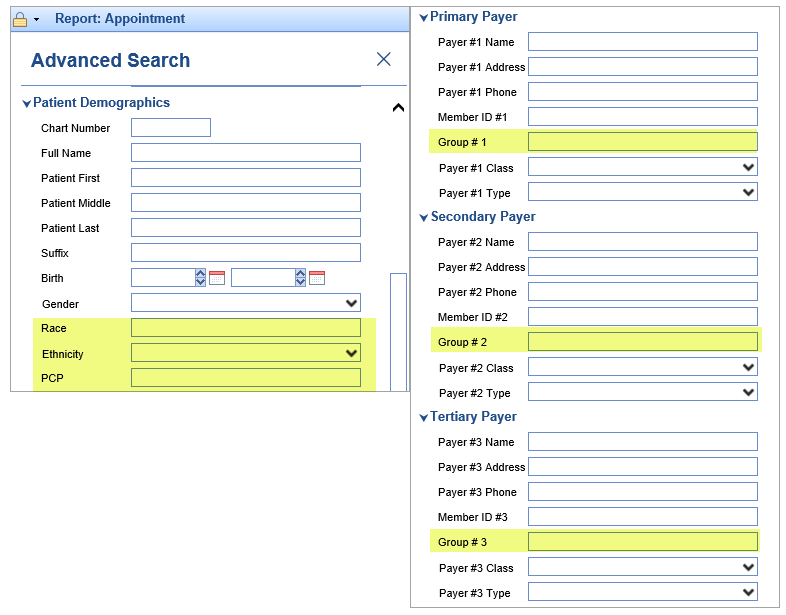
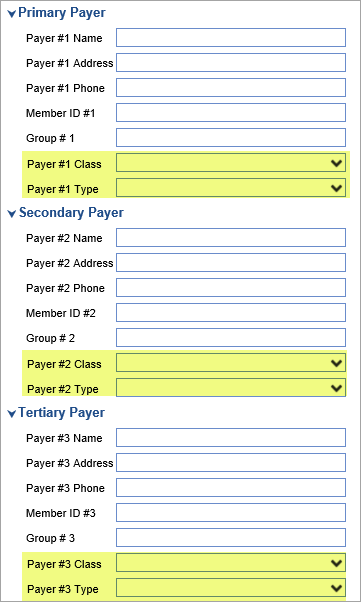
- U11679, U11686 - Added additional Payer search fields: Added Primary, Secondary, and Tertiary Payer Class and Type fields to the Advanced Search screen along with Primary, Secondary and Tertiary appointment flags of the Appointment report:
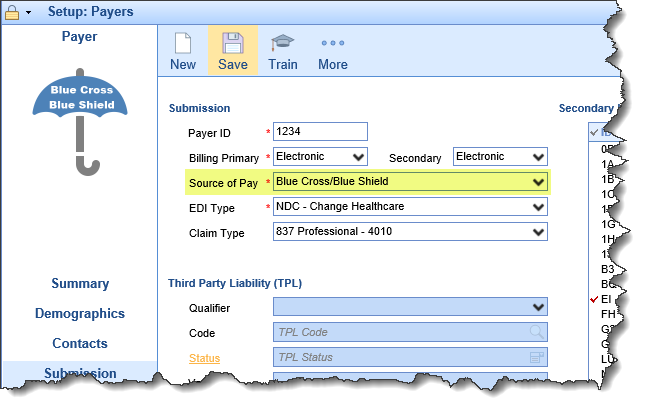
 This information will be based on the Source of Pay that is selected in the Payers Setup screen:
This information will be based on the Source of Pay that is selected in the Payers Setup screen: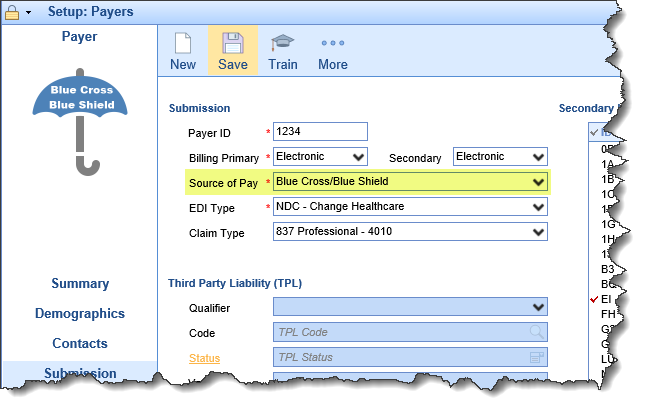 Note: These fields will not display in the report by default. In order to display, they must be enabled in the More > Change Display Settings menu:
Note: These fields will not display in the report by default. In order to display, they must be enabled in the More > Change Display Settings menu: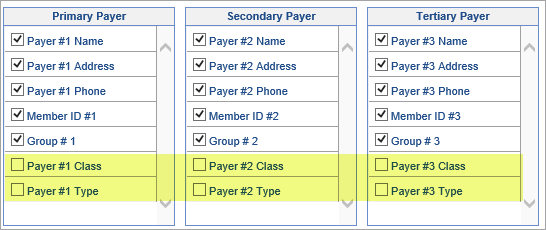
EMR
Summary
- B11531 - Scrolling issue with Lab Results: When launching Lab Results from the Summary Timeline the results would not open in a full window. This forced users to have to scroll in order to see all of the data. This issue has been resolved.
Order Entry
- B11048 - Order Fulfillment and AOE questions not displaying on Requisition for some orders: When using the search feature to find orders, Fulfillment information and AOE questions added to that order were not displaying on the Requisition. This issue has been resolved.
Letters
- B11471 - Template default values not respecting carriage returns: When custom quick picks for Letters and Bluebars were used in a template, any default values that contained carriage returns (extra line spacing) would not display correctly on the Letter. This issue has been resolved.
Billing
Receipts
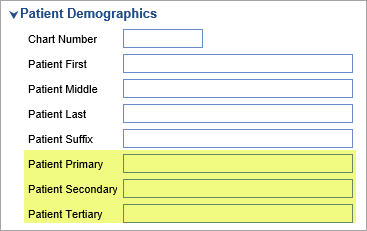
- U11476 - Added additional search fields to Receipts Search: Added Patient Primary, Patient Secondary, and Patient Tertiary to the Advanced Search screen within the Receipts window.
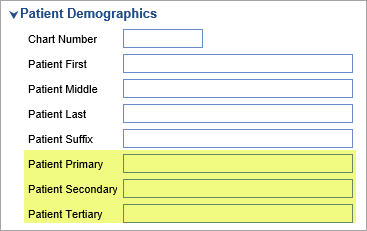 Note: These fields will not display in the Receipt search results by default. In order to display, they must be enabled in the More > Change Display Settings menu:
Note: These fields will not display in the Receipt search results by default. In order to display, they must be enabled in the More > Change Display Settings menu: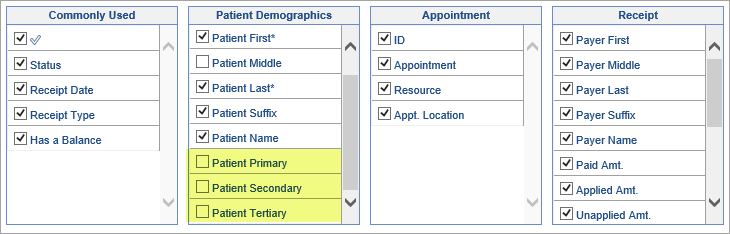
Reports
- U11621 - New 'Lost to Followup' report: Created a new report called 'Lost to Followup.' This report will assist Practices in identifying patients who have received services and meet certain problem list criteria, but who don't currently have further appointments scheduled. For more information on adding and running this report, click here.
- U11028 - New 'CCM Missing Consent Dates' Connect report: Created a new Connect report called CCM Missing Consent Dates which returns patients who are actively receiving Case Management services but are missing a verbal consent date. For more information about using this report, click here.
- U11532 - New 'CCM Status Changes' Connect report: Created a new Connect Report called CCM Status Changes which uses the parameters: Client, Start Date, End Date, Starting Status, and Ending Status. For all selected CCM clients over the range specified it then finds the number of daily status changes from one of the selected starting/ending statuses, which is then divided out by the users who changed the statuses.
- U11737 - Added drill-through functionality into the new Billing Analytics package: Defined a drill-through view for several measures. This will allow users to drill into those measures in order to see formatted detail information.
Claims
- B10984 - Authorizations inconsistent between Appointment and Claim: Resolved an issue in the authorizations process where the Claim and Appointment could diverge in terms of which authorizations were attached. Now, if a Claim is created from an Appointment with an authorization, the authorization will be attached to the claim as well. In addition, any changes made to the Appointment authorization will be mirrored on the claim and vice versa.
 This information will be based on the Source of Pay that is selected in the Payers Setup screen:
This information will be based on the Source of Pay that is selected in the Payers Setup screen: