MSP stands for Medicare Secondary Payer. When another insurance is primary over Medicare, Medicare wants to know why. An MSP Reason is the way we transmit that information on an electronic claim.
NOTE: Not including the MSP Reason on a claim will cause secondary claims sent to Medicare to reject.
- To set or change an MSP Reason, you will need to go into the Patient Insurance Setup screen, and select the reason from the drop down menu. You will not be able to select an MSP reason until after Medicare has been saved as an insurance in the Patient Insurance Setup screen.

- There are nine valid, Medicare approved options for the MSP Reason:
MSP Insurance Type
MSP Provision
iSalus Terminology
12
Working Aged – Beneficiaries age 65 or older who are insured through their or their spouse’s current employment. Employer’s group plan has 20 or more employees.
Note: This type must only be used for beneficiaries who are 65 years old or older on the date the service was rendered.
Employer Group
13
End Stage Renal Disease (ESRD) – Beneficiaries enrolled with Medicare solely due to renal failure and are insured through their own, or through a family member’s former or current employment. Medicare is the secondary payer for the first 30 months from the beneficiary’s Medicare eligibility date.
Note: This type is not age specific.
ESRD
14
Automobile/No Fault – No-fault insurance that pays for medical expenses for injuries sustained on the property or premises of the insured, or in the use, occupancy, or operation of an automobile regardless of who may have been responsible for causing the accident.
No-Fault Insurance
15
Workers’ Compensation – Insurance that employers are required to provide to cover employees who become sick or are injured on the job.
Worker’s Compensation
16
Federal Agency (Public Health) – Services that are the direct obligation of another Federal, State or Local Governmental entity.
PHS or Other Fed. Agency
41
Black Lung – Coverage under the Federal Black Lung Program due to black lung disease and other respiratory conditions caused by coal mining in which a Medicare beneficiary may be entitled to have services reimbursed by the United States Department of Labor (DOL).
Black Lung
42
Veterans Administration – A federal program supervised and supported by the Department of Defense that provides medical coverage benefits for beneficiaries who were members of the Armed Forces. Veterans who are Medicare-eligible may elect whether Medicare or VA benefits will handle their claims.
Veteran’s Administration
43
Disability – Beneficiaries under age 65, who are disabled and insured through their current employment or through the current employment of a family member. Employer’s group plan has 100 or more employees.
Note: If the basis of disability is ESRD, the ESRD type should be used when billing Medicare. Also, the Disability type must only be used for beneficiaries who are under 65 years of age on the date the service was rendered.
Large Group Health Plan (LGHP)
47
Liability – Insurance (including a self-insurance plan) that provides payment based on the policyholder’s alleged legal liability for injury or illness or damage to property. It includes homeowner’s liability insurance, malpractice insurance, product liability and general casualty insurance and payments for medical damages made under the “wrongful death” statutes.
Other Liability Insurance
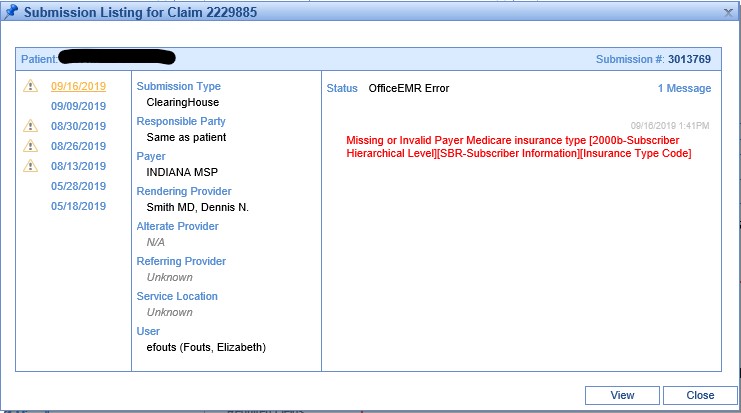
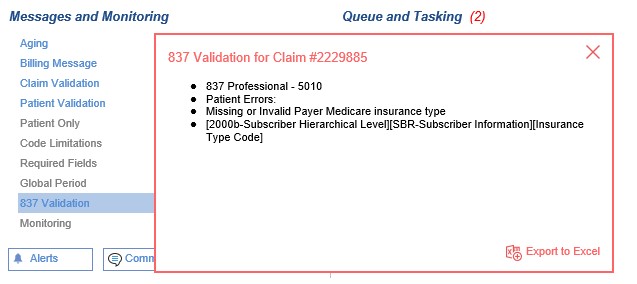
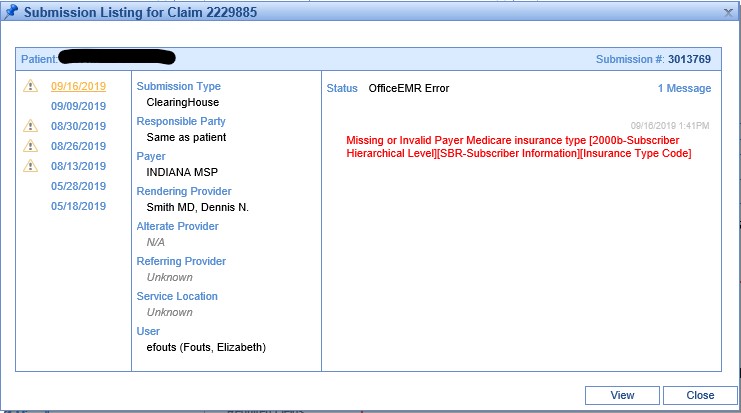
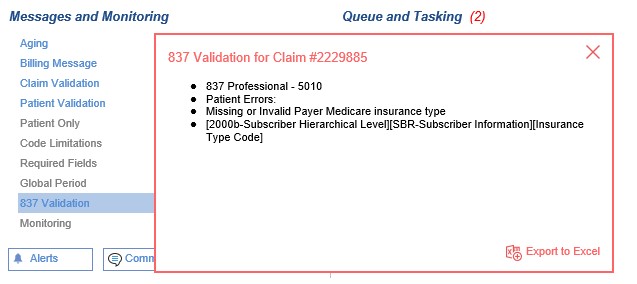
- If an MSP Reason is not selected, claims submitted where Medicare is the secondary payer will be rejected. This rejection detail will be visible in the View Submission History, or in the Messages and Monitoring section in the Claim Detail. The 837-5010 EDI claim format refers to the MSP as an Insurance Type Code, as seen in the rejection.