New Features
General
Timezone
- U9171 - Added the ability to display timestamps in any timezone format: Since our clients utilize our software in various time zones (MST, EST, PST, CST) we have added the ability to customize how times are displayed in the system for that user. The new timezone logic will display the timezone based on the priority described below.
- The default setting will be based on the zip code that is configured in the Company Profile (Settings > Company Profile):
- The timezone can also be configured by user. If a user has their own timezone configured then this will override the Company Profile setting above. Learn more about this user setting here: User Setting: Timezone Zip Code
Please note, we will be rolling this new feature out to specific sections of the software with each release. With this release, the newly configured timezone as been added to the following places:
- My Tasks
- Superbill
- SOAP Notes
- eDocuments
- Patient Portal
- Health Exchange
- Case Mgmt
- NYSED
- Pop Health
Billing
Deposits
- U9800 – Improved accuracy of payer on deposits: Deposits will no longer load a payer if there is more than one match for the received payer ID. In the process of auto-linking deposit claims to claims in the system, if the deposit payer is blank then it will be auto-populated from the first linked claim.
- U9745 – Created error for ERA payment lines with no amounts listed: When posting a deposit claim, the system will check to see if on any given line the paid and allowed amounts are $0 + no CARC codes have been added + the Charge amount is greater than $1. If this is the case, it’s likely that the payer has neglected to send some sort of key information, and a claim error will triggered. This error lets the user know that this has occurred and prompts them to set the resulting claim level and status as desired.
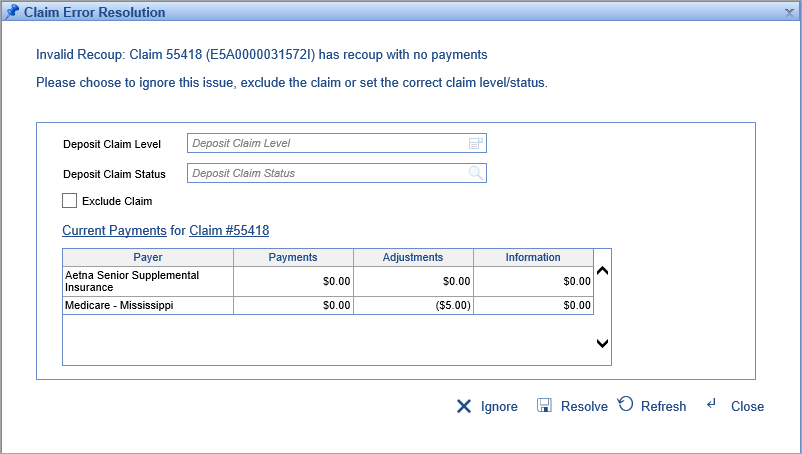
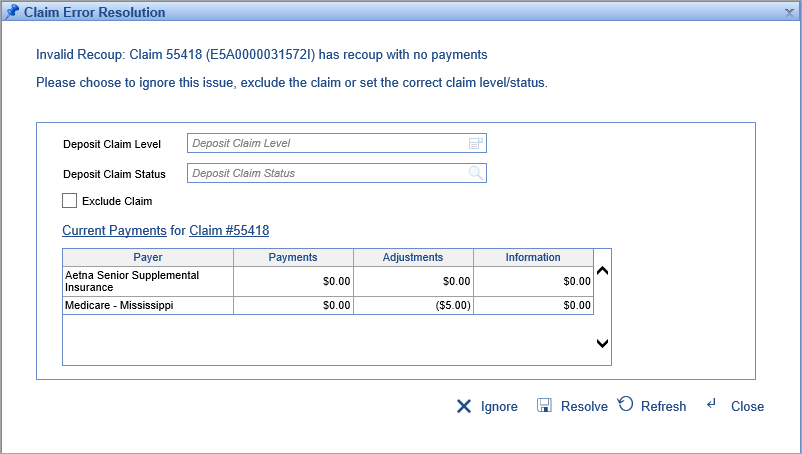
- U9653 – Created error for recoups with no originating payments: Sometimes a payer will send a payment and a recoup for that payment in the same ERA. In those instances, if the recoup was listed before the payment then the system would post the recoup first and then the payment second. Because the payment would look like a full payment, the status/level would be set as if the line was paid even though the payment had already been recouped. To resolve this, we have created a claim error that triggers when a recoup is being posted with no originating payment from the same payer. This will ‘hold’ the posting so that it can occur after the associated payment, which will allow the user to set a different resulting claim level/status if needed. Learn more about this error here: Invalid Recoup
- U9634 – Modified posting process to handle full CO-45 adjustments: It’s possible for payers to adjudicate a billed amount by writing off the full amount as a contractual adjustment (which is effectively a denial.) However, in this situation many systems won’t trigger processes for handling denials. To resolve this scenario we have added two new company settings called Full Contractual Adjustment Claim Status and Full Contractual Adjustment Payment Type. These values will be used in lieu of the normal CO-45 settings if the contractual adjustment amount on an ERA line equals what the ERA has listed as the line’s total charge amount. By default, these values are set to:
- Full Contractual Adjustment Payment Type = [ERA No Payment]
- Full Contractual Adjustment Claim Status = [Denied]
- U9627 – Modified posting process to ignore adjustments on denied lines: Often when payers deny a certain procedure, they will send a denial for the full charge amount of the line. However, occasionally certain payers will send a contractual adjustment writing the procedure down to the allowed amount, and a denial for only the allowed amount. This can cause extraneous adjustments if the payer then re-sends the contractual adjustment with the eventual payment as well. In order to handle situations such as this, we have created a new company setting called No-pay Denial Payment ID. Now, on any line that is receiving a CARC code with the Denial flag checked, all other CARC codes on this line will be set to the payment type from this company setting. By default this value will be set to:
- No-Pay Denial Payment ID = [ERA Information Only]
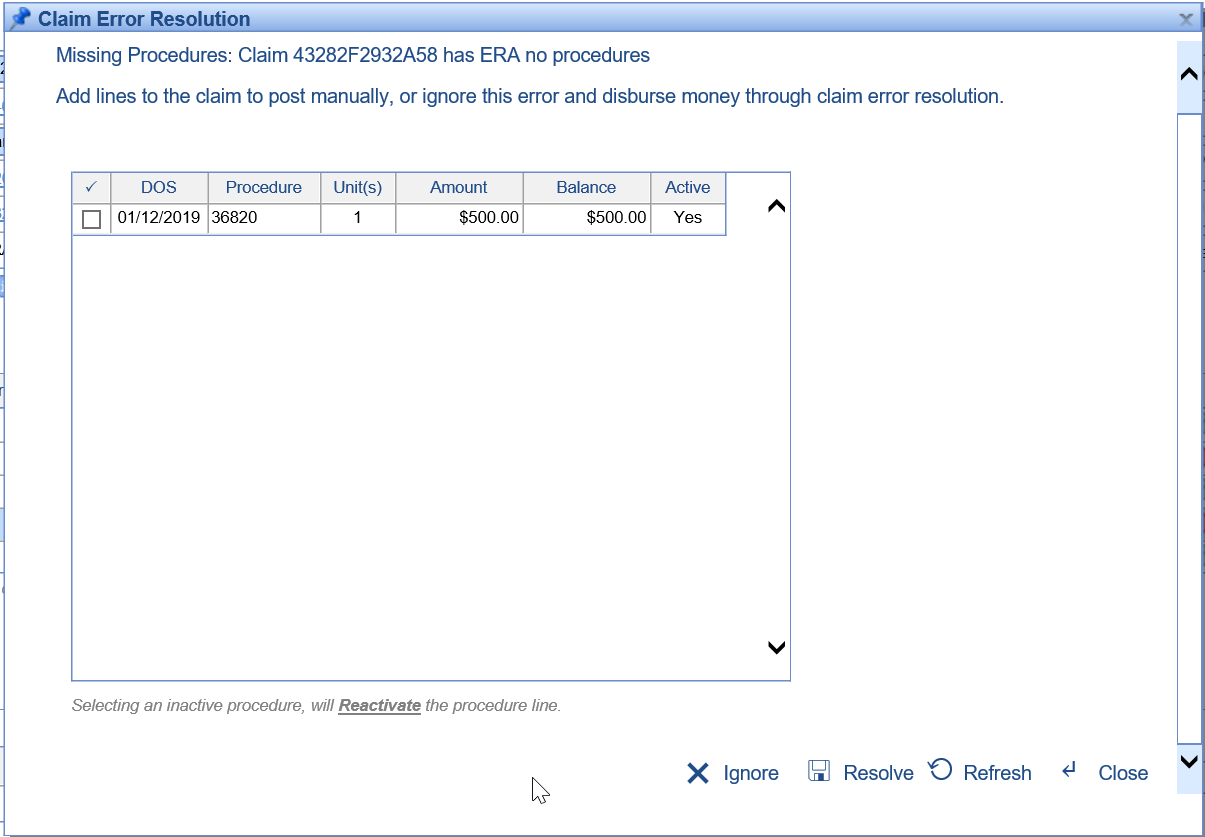
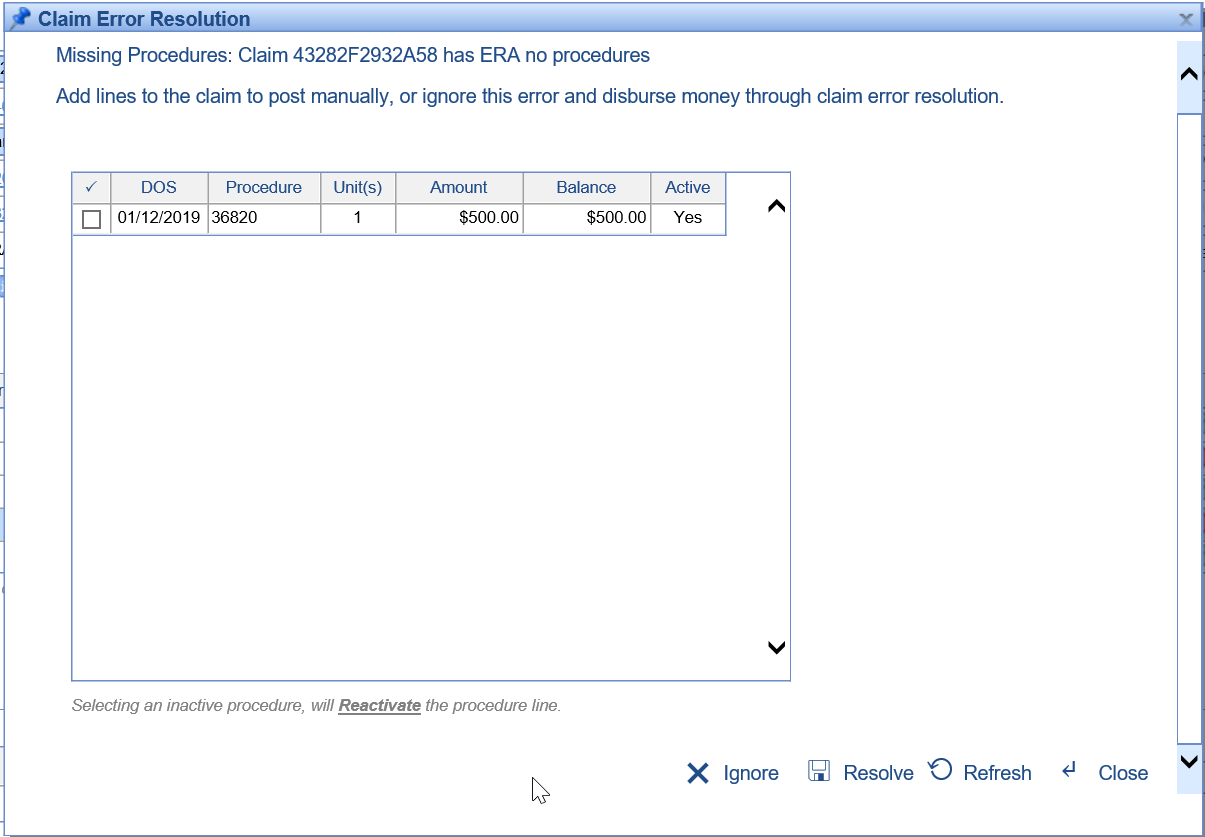
- U9545 – Created error for deposit claims with no procedure lines: When an ERA is being processed, the system will now check to ensure that a given deposit claim has procedure lines on it. If it doesn’t then the system will trigger a claim error with options to add procedures from the claim. Learn more about this error here: Missing Procedures
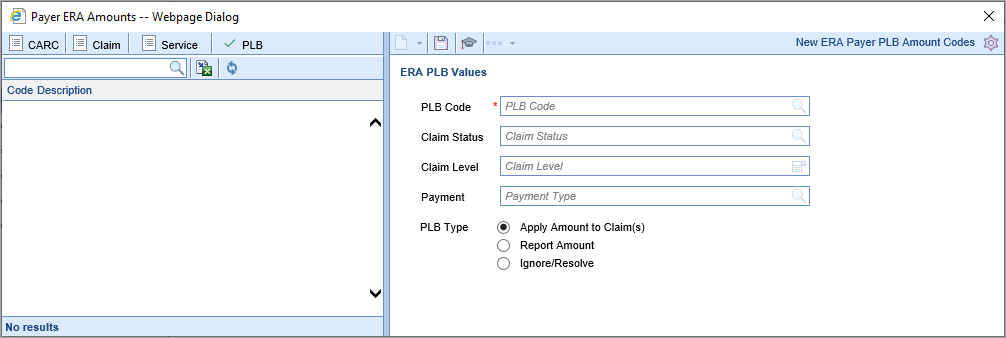
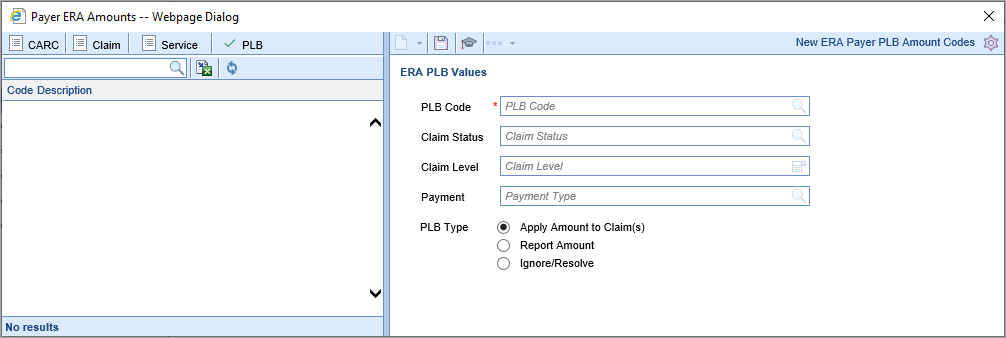
- U9544 – Created payer overrides for PLB and Service Amounts: Previously, at the payer level users could override the decision to ignore certain PLB codes. This change adds granularity to these payer-level overrides, allowing users to extensively customize how the system typically handles CARC, Claim, Service, and PLB amounts...and then how individual payers may need to handle them differently. The payer-level setting will always be used first if it exists - if not, the general setting is used. Learn more here: ERA PLB Amounts
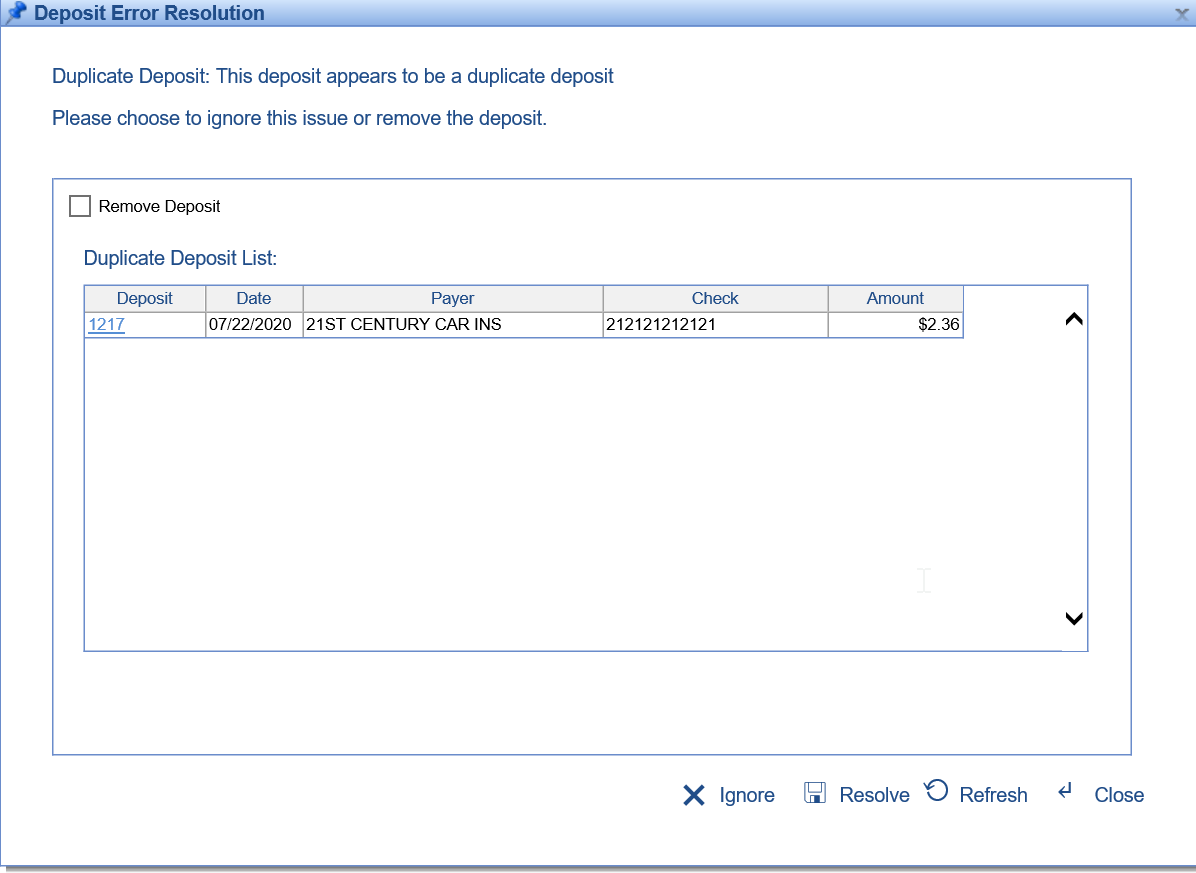
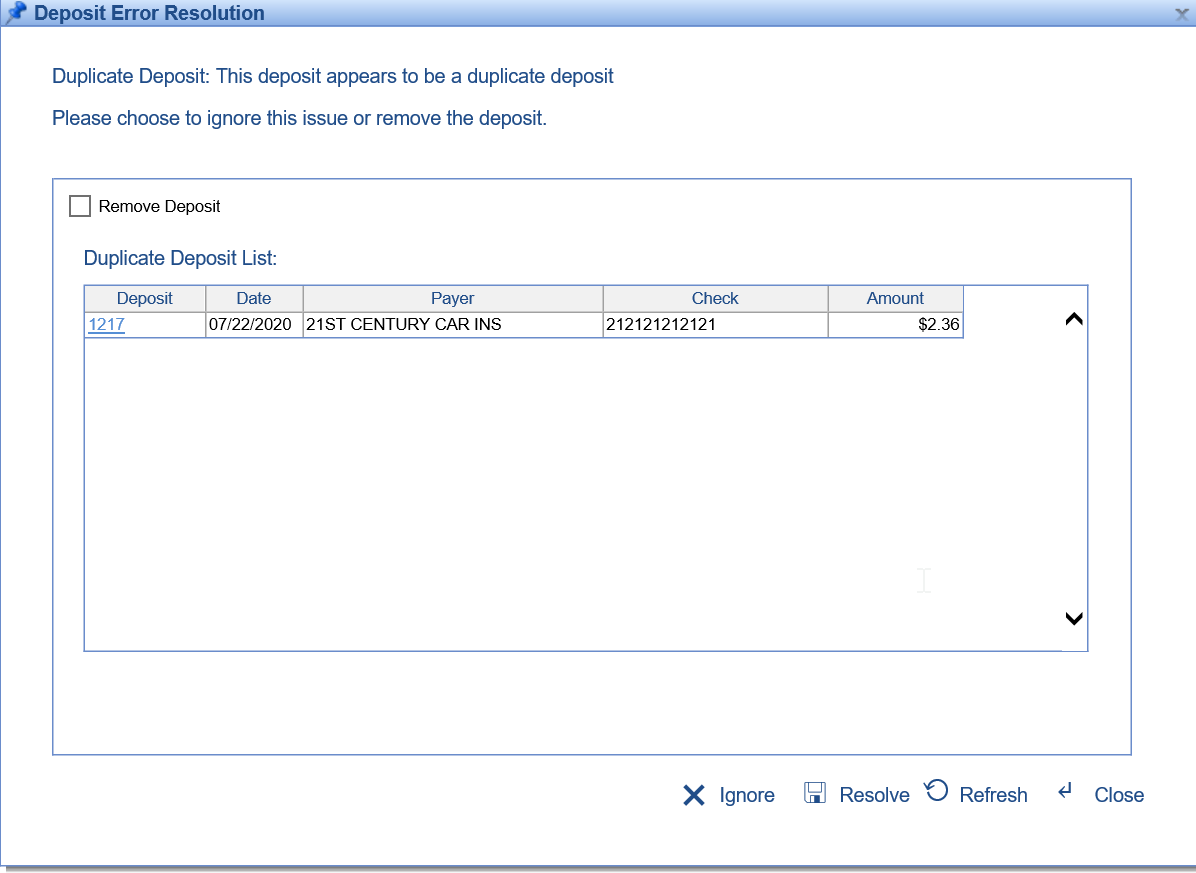
- U10210 - Added logic to check for duplicate EOB deposits: Whenever an EOB is created, the system will now check for an existing deposit that may already be in the system. The match will be based on Deposit Date, Check Amount, and Check ID. If a duplicate deposit is found, then a deposit error will be added to the deposit. Learn more about this error: Duplicate Deposit
Updates and Bug Fixes
My Tasks
- B10166 - Error when clicking on Lab Results: Resolved an issue where some Lab Results would display a 'web service' error when clicking on them. Note: Since this only addresses new Lab Results, users may still experience an error with pre-existing Lab Results. Please contact a Customer Care team member if you are still encountering errors.
EMR
Problem List
- B10229 - Notes were overlapping the Diagnosis: Resolved an issue where in some instances the Notes would overlap the Diagnosis when viewing the Problem List in 'Text' format (this only occurred when using IE):

Billing
Setup
- U10077 - Made Receipt Indicator and Credit Indicator editable for all payment methods: Both Receipt Indicator and Credit Indicator can now be edited for all Payment Codes. These were originally being locked down if the payment type had been used.
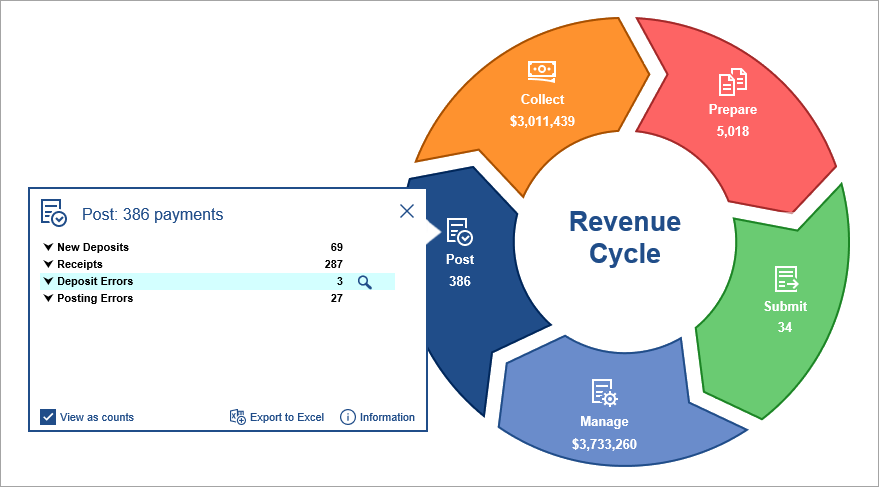
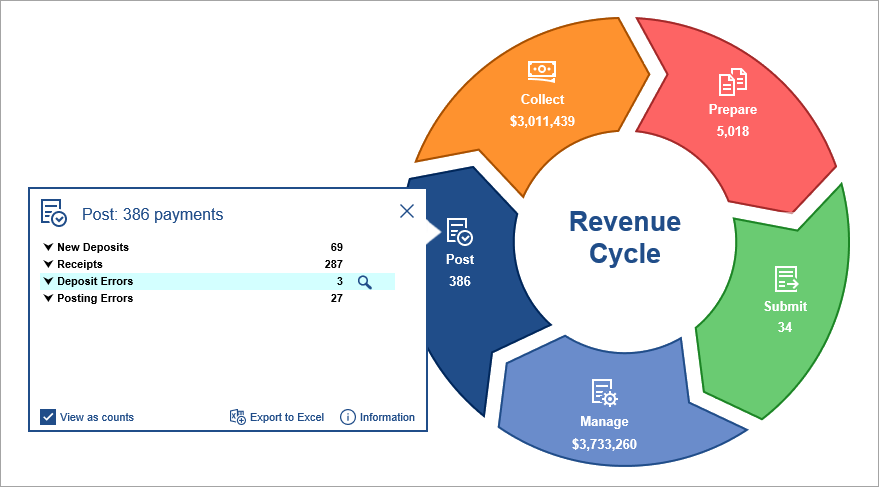
Revenue Cycle Wheel
- B10219 - Updated the filter on the Deposit screen when launched from the Billing Wheel > Deposit Errors: Resolved an issue where when clicking Deposit Errors from the Billing Wheel, the resulting Deposit screen was erroneously filtering out Deposits that had a Status of 'Sent to Posting'.
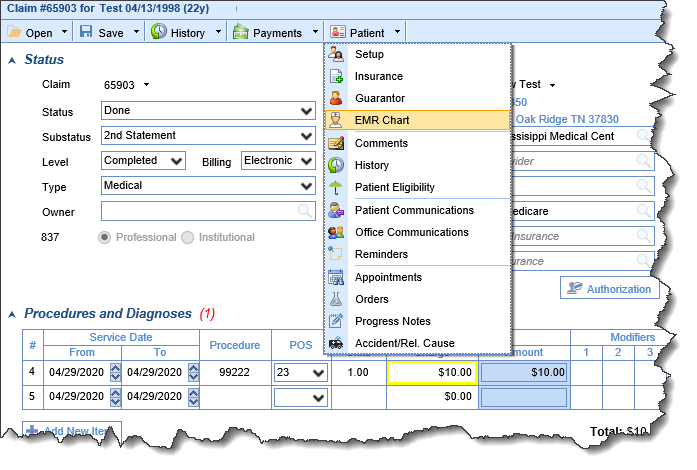
Claims
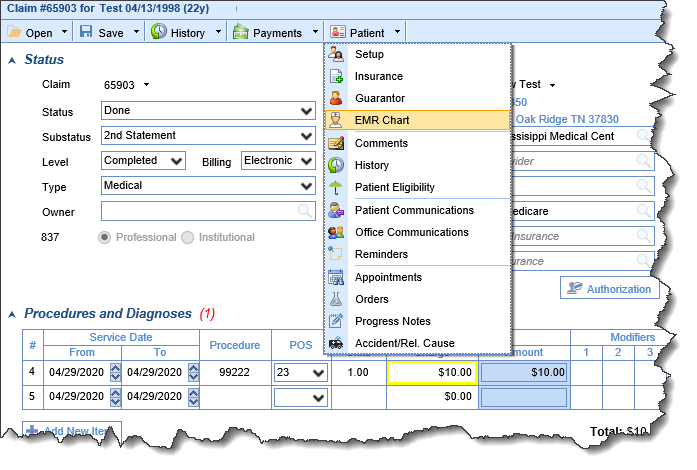
- U10209 - Added the ability to open a patient in EMR from the Claims screen: From within the Claim details screen, users now have the ability to launch a patient directly in EMR using the EMR Chart option from the Patient drop-down menu:
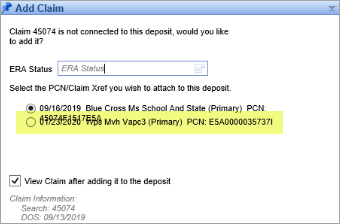
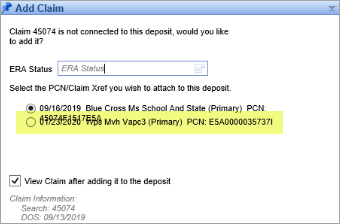
- B9898 - Lines overlapped on the Add Claim window: Resolved an issue where if the Primary Payer had a long name and the Secondary had also already been sent, then the two lines would overlap on the Add Claim window:
- B10009 - Duplicate Claim message was not displaying the correct claim number if it ended in '0': When adding multiple claims to a deposit, the duplicate claim message that was displayed was dropping the last digit of the claim number if the claim number ended in '0