Denied claims are claims that have been adjudicated by the payer and have received an EOB Denial. Denied claims require that the user review the deposit and or Human Readable ERA to determine the cause of the denial. Once the denial reason is corrected the claim must be resubmitted to the payer.
Workflow
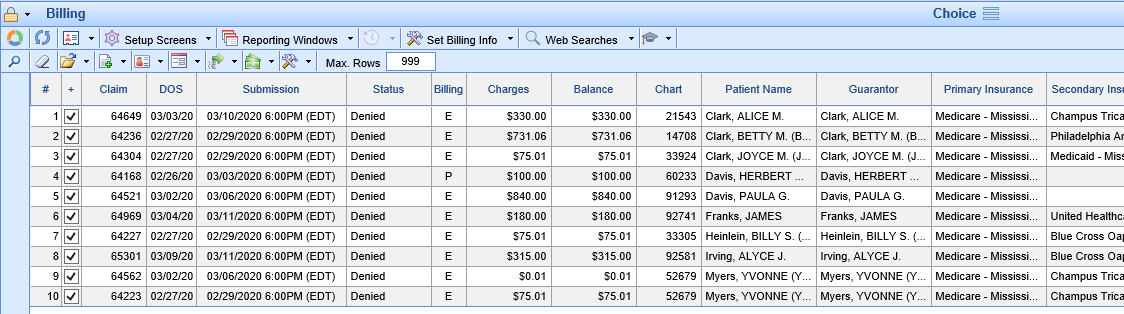
- Click the magnifying glass to open Billing Query.
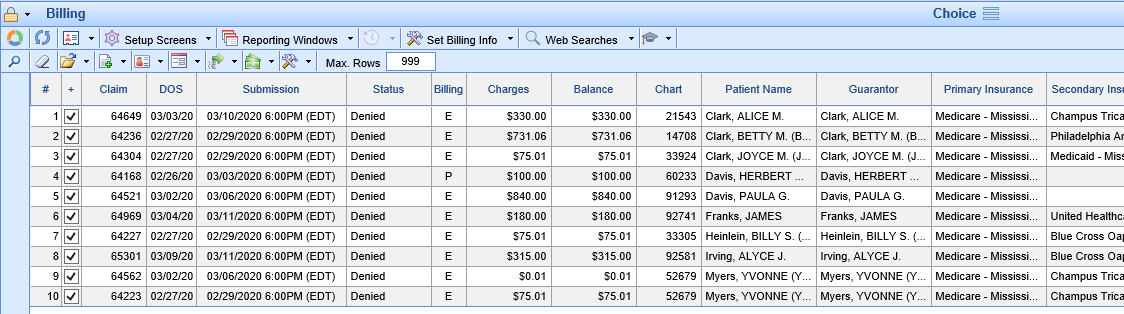
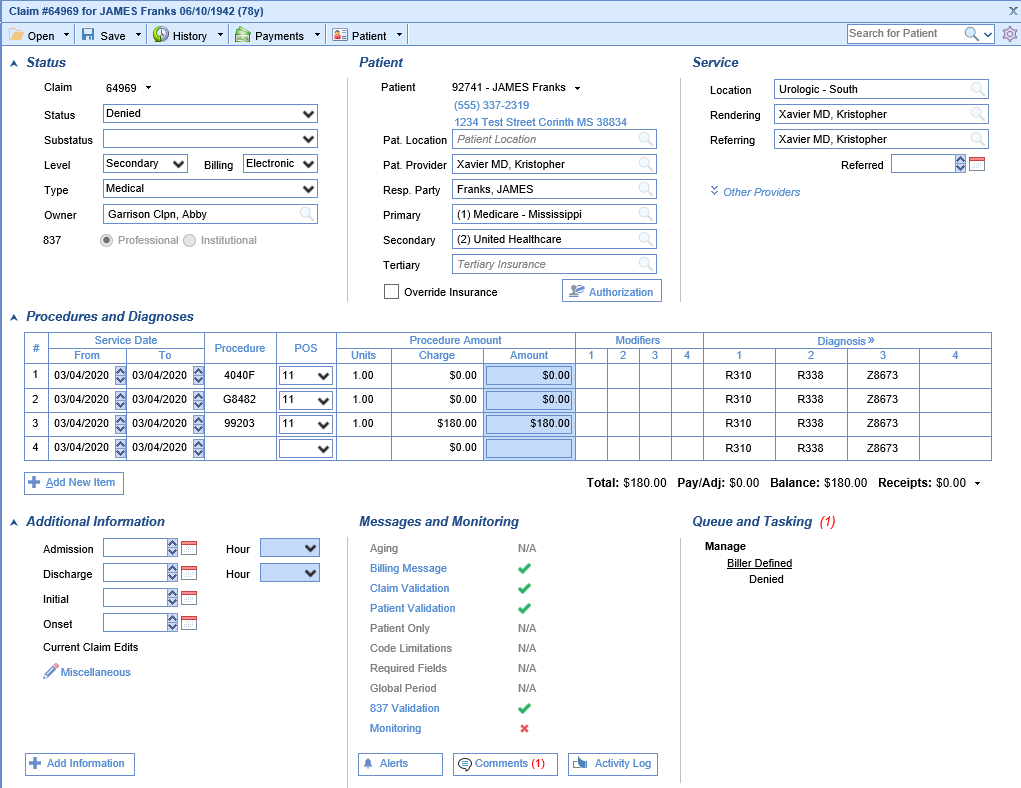
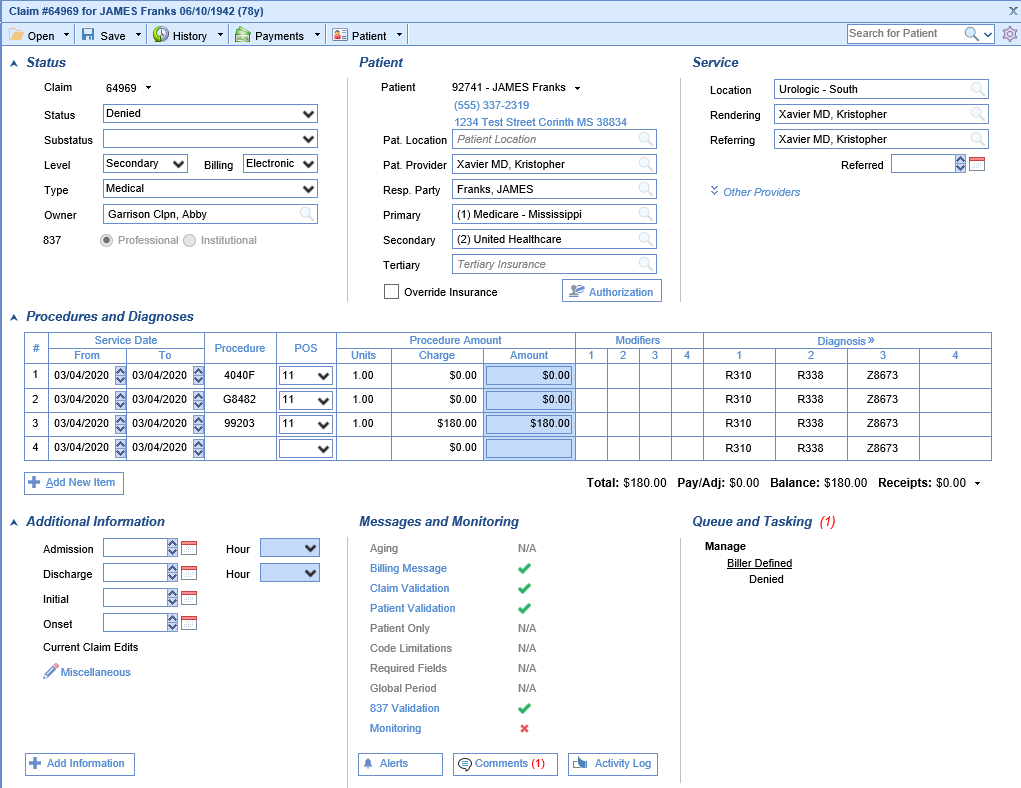
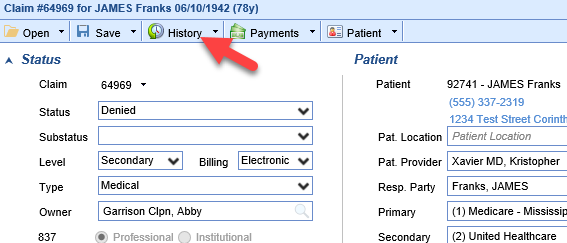
- Double click the claim to open the Edit Claim screen. Review the claim to determine the reason the claim is in a denied status.
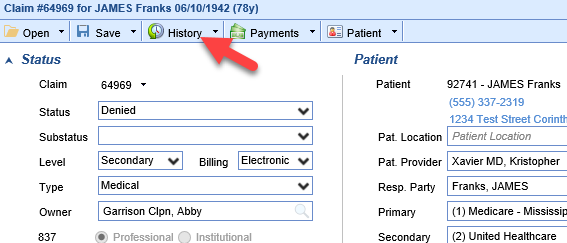
- Click on the History button at the top of the screen.
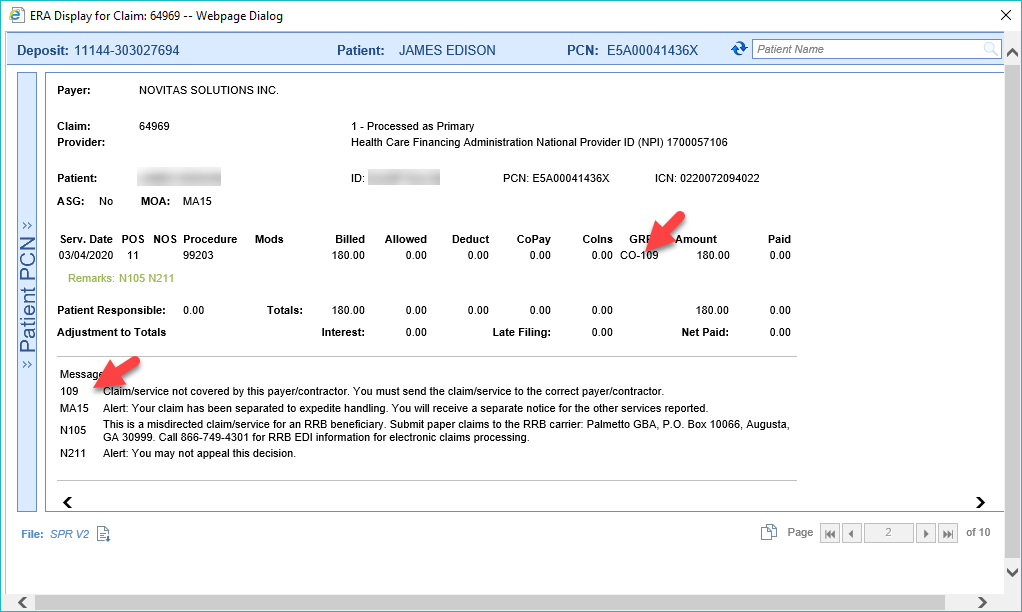
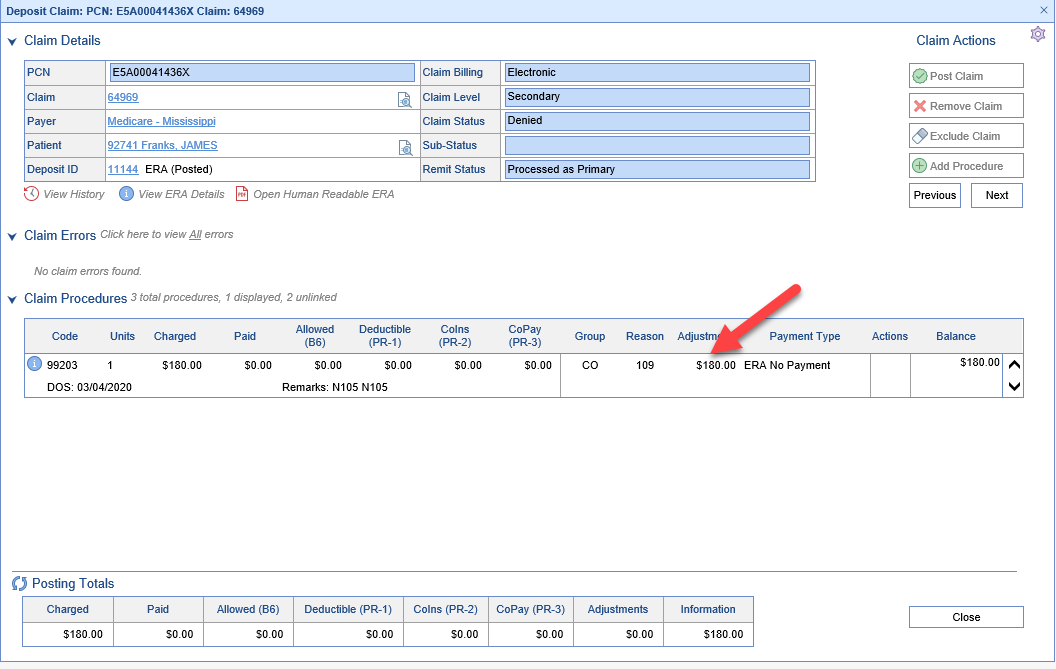
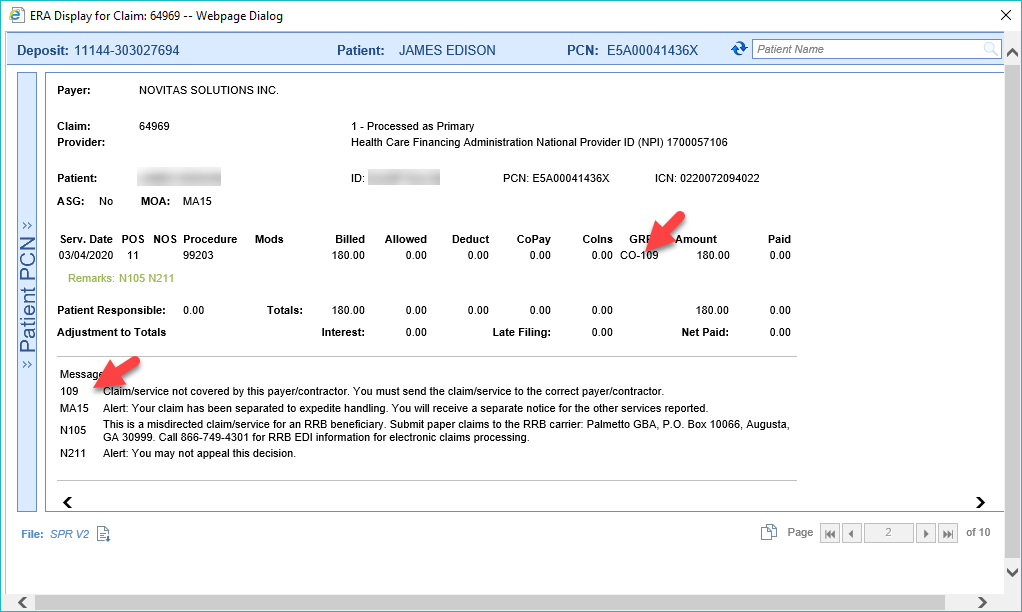
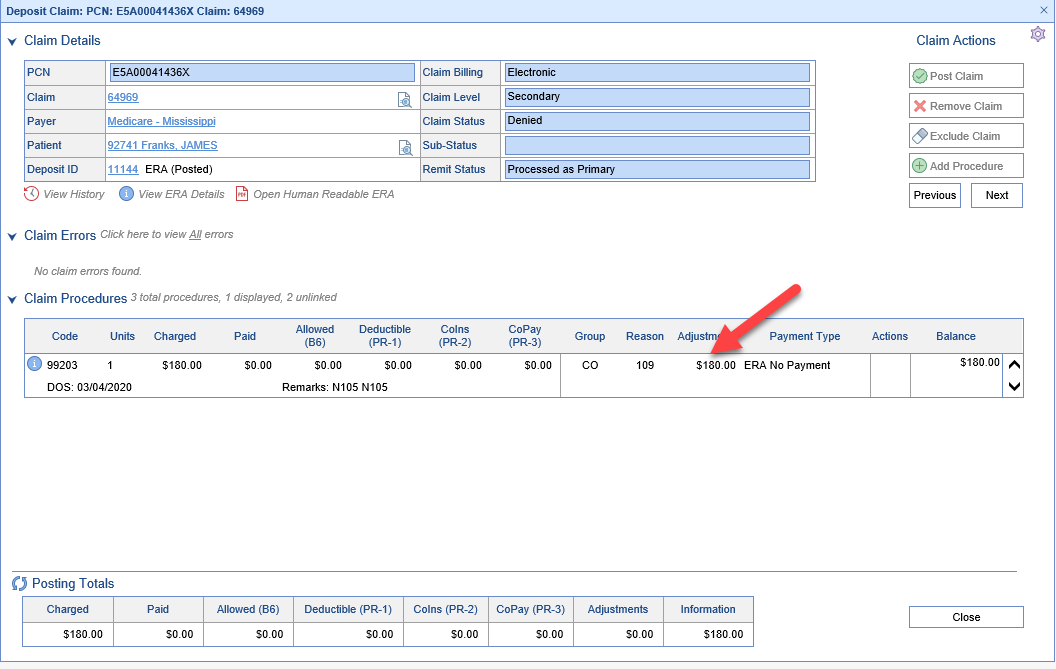
- Right-Click on the payment and Select ERA or Deposit to view the Denial Reason
- ERA
- Deposit
- ERA
- Depending on the denial reason, either
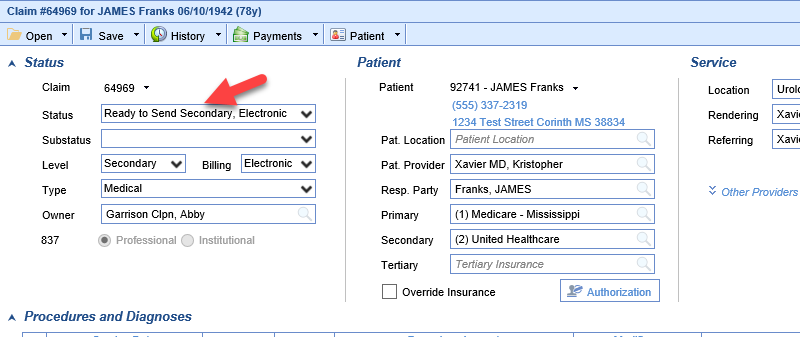
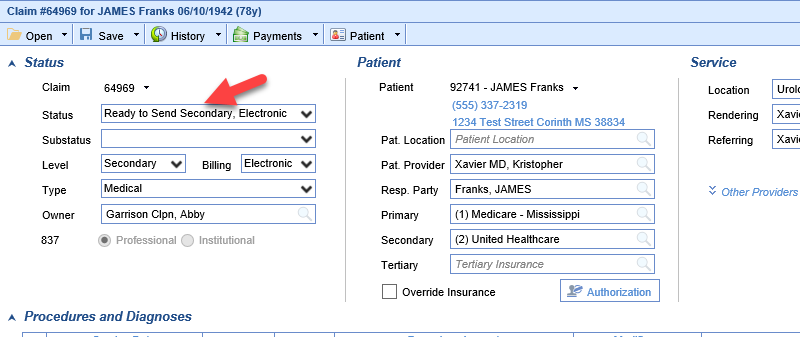
- Make the correction to the claim and update the claim status to Ready to Send
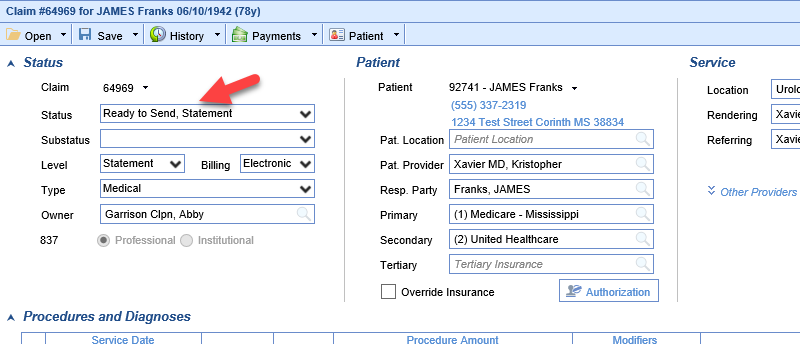
- Bill the patient
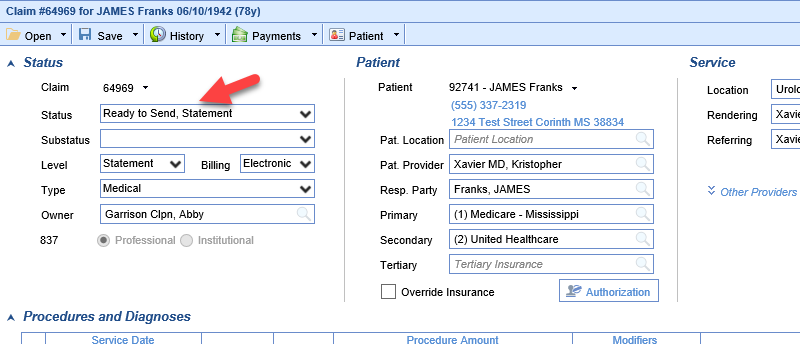
- Write-off the balance of the claim
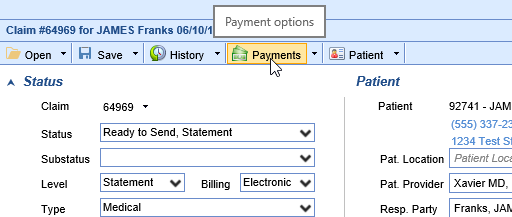
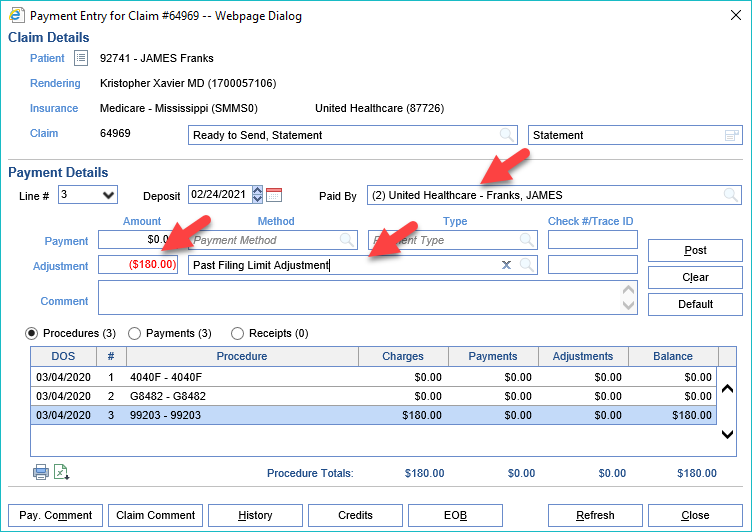
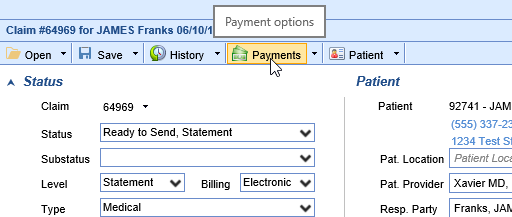
- Click Payments
- Enter the Adjustment information
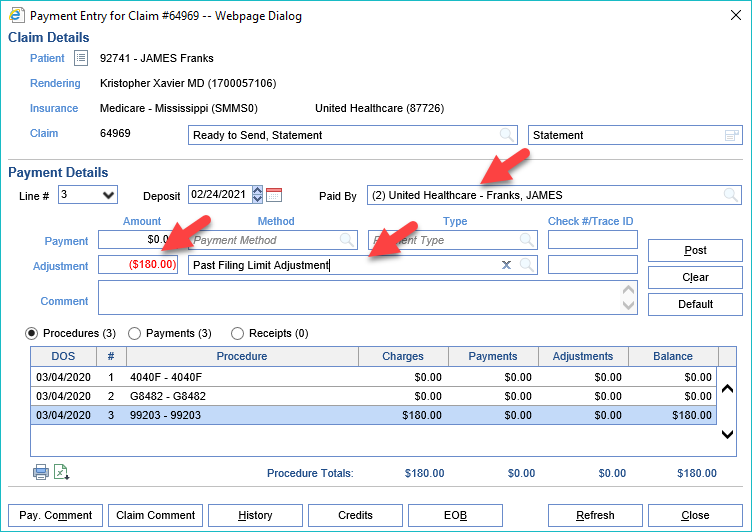
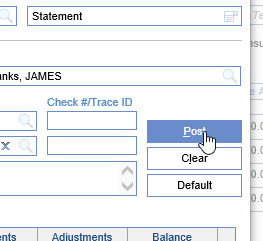
- Click Post
- Click Payments
- Make the correction to the claim and update the claim status to Ready to Send