Question: One of our claims has rejected for "Line Level Procedure Code is Missing or Invalid". How do I fix this rejection?
Solution: There are several situations when this can happen:
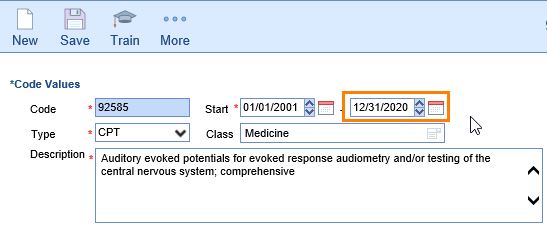
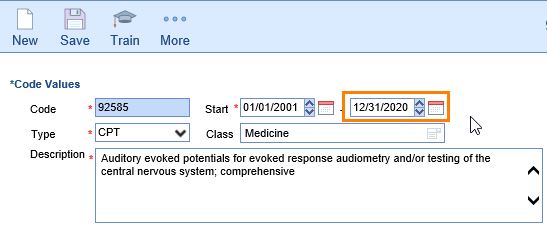
- Verify that the procedure code(s) are valid codes in the current billing year. If the code is no longer valid, a user should go in and put in an Effective End Date for the code.
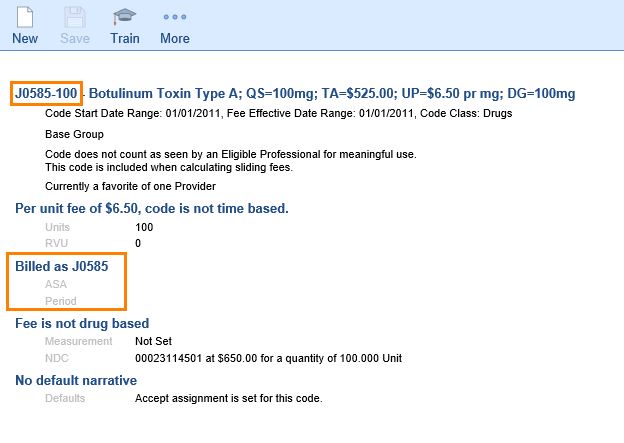
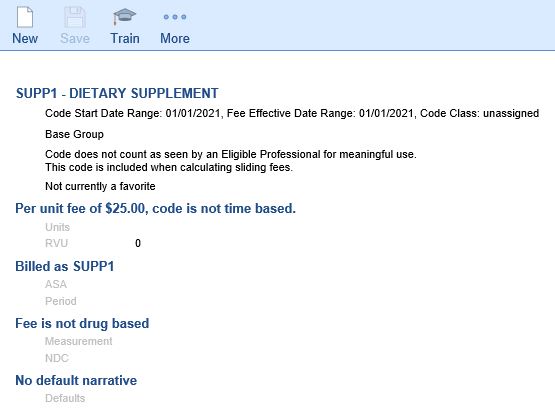
- Verify that a procedure code has a valid Billing Code. Sometimes various "modified codes" are used for reporting, default modifiers, etc. However, a valid CPT/HCPCS code will need to be entered in the Billing Code field.
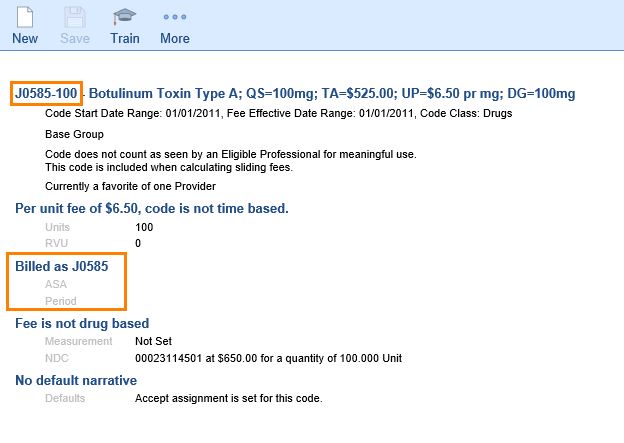
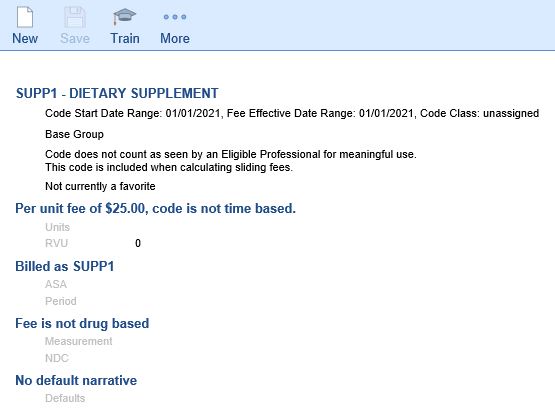
- Verify that a procedure code has a valid CPT/HCPCS equivalent. A practice may create "dummy codes" for internal tracking purposes, which were never intended to be submitted to insurance. Rejected claims in this category will need to be switched to Ready to Send Statement status with a Statement level, or adjusted.
If none of these situations appears to apply, please contact the Customer Success team at iSalus Choice for assistance.