This screen will query the database to determine all accounts that have claims with a credit balance. It will also check total patient balances for the patients who have claims with credit balances. Each line is a summation grouped by patient.

Fields
These are found under More > Change Display Settings
Chart Number: The unique number assigned to a patient account
Patient Name: The patient name for the account with claims containing a credit balance.
Transferable: If there is a credit balance and a corresponding claim with a positive balance, an icon will appear here to denote that.
Credit Balance: The sum of all balances of claims with a credit balance.
Open Balance: The total balance of the account.
Patient Balance: The total balance of the account that's currently at patient responsibility.
Patient Refunds: Claims with refund balances set to Claim Status = Refund and Level = Patient.
Insurance Refunds: Claims with refund balances set to Claim Status = Refund and Level = Primary, Secondary or Tertiary.
- Next Appointment: The date of the next appointment for the patient.
Resp. Party EID: The entity identification number assigned to the Responsible Party
Resp. Party Name: The name of the responsible party listed on the account with claims containing a credit balance
Provider ID: The system identification number assigned to the Provider
Provider Name: The Provider name for claims containing a credit balance
Location EID: The entity identification number assigned to the Location
Location Name: The location name for claims containing a credit balance
Toolbar

- Open: Opens Claim Credit Select Window
- Train: Opens link to iSalus' Help Center
- More: Provides links to Change Display Settings and the Refund Register Search
Screen View Checkboxes
- Patient Refund: Check this box to ONLY see refunds set to patient
- Insurance Refund: Check this box to ONLY see refunds set to insurance
- Check both boxes to see accounts with refunds set to BOTH patient and insurance
- Uncheck both for accounts that contain either patient refunds, insurance refunds or unassigned refunds
- Top 100 Highest Credit Balances: This is set as the default selection to display the highest credit balances for working and prevent slowness on the screen.
- Top 100 Lowest Credit Balances: User can see the lowest credit balances instead.
Gear Icon
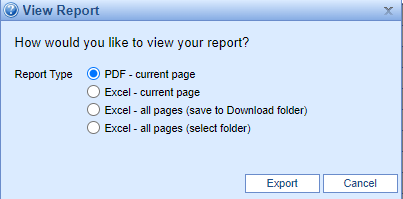
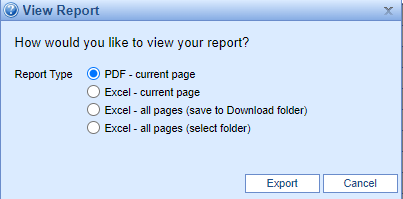
Print: Clicking this button will print the credit balance selection results as a report.
PDF: Clicking this button will create a pdf preview of the results report.
Excel: Clicking this button will create an Excel export of all items in the current search results containing all fields listed on the screen.
Advanced Search Fields
- Chart Number: A field to search for a single patient's credits.
Transferable: NA/Yes/No. Filter will allow the user to only see items that are/are not transferable.
Credit Balance: The minimum and maximum credit balances to display.
Open Balance: The minimum and maximum open balances to display
Patient Balance: The minimum and maximum patient balances to display
Patient Refunds: The minimum and maximum patient refunds to display
Insurance Refunds: The minimum and maximum insurance refunds to display
- Patient First: Search by patient's first name.
Patient Middle: Search by patient's middle name.
Patient Last: Search by patient's last name.
Patient Suffix: Search by patient suffix.
Next Appt.: The date of the next appointment for the patient
Resp. Party EID: The entity identification number assigned to the Responsible Party
Resp. Party Name: The name of the responsible party listed on the account with claims containing a credit balance
Provider ID: The system identification number assigned to the Provider
Provider Name: The Provider name for claims containing a credit balance
Location EID: The entity identification number assigned to the Location
Location Name: The location name for claims containing a credit balance
Remember some fields are searching for negative balances. If searching for credit balances between -$100 and -$1000, enter it as -1000 to -100 
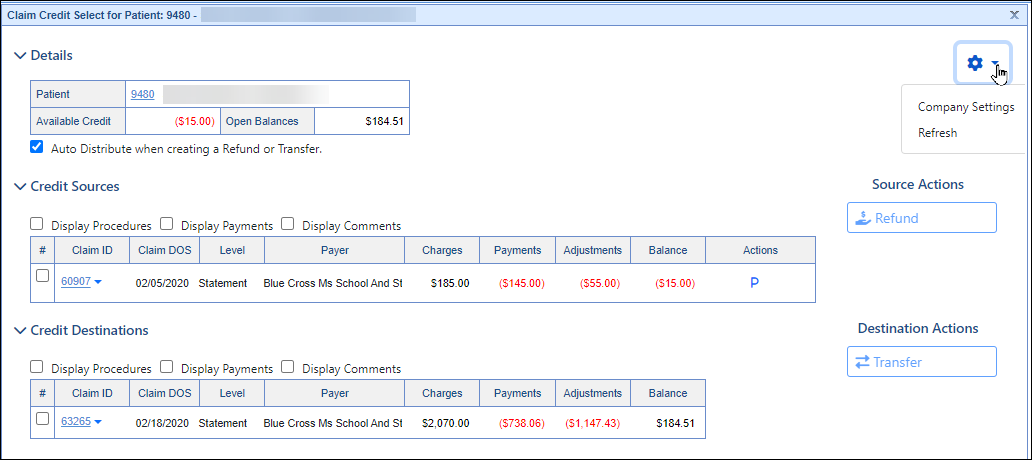
Claim Credit Select
Clicking on any part of the line on the Credit Balance screen brings up the Claim Credit Select window.
The basic purpose of this screen is to
Approve sources for patient or insurance refunds
Select source credits for a refund or transfer
Select credit destinations for transfer
Fields
Details
Patient: The account number and name of the patient with the credit balance. Link to open Patient Setup by clicking the Account number
Available Credit: The total amount of the available credit balances.
Open Balances: The sum of the claim balances available for transfer.
Auto Distribute when creating a Refund or Transfer: If checked, on the next screen the system will allocate the selected credits across selected Credit Destinations. If unchecked, the screen will start with no money allocated.
Credit Sources
These are the available selections to choose the credit sources for your transfer. The information shown will look similar to information as shown on a statement, to help the user make the best determination as to what needs to happen with the credit. It will contain the following information:
- Checkboxes:
- Display Procedures: Procedures will be displayed for all claims listed
- Display Payments: All payments toward claims will be displayed for all claims listed
- Display Comments: All comments will be displayed for all claims listed
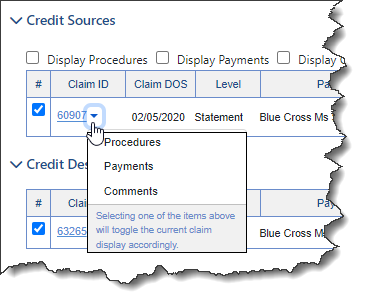
Claim ID: The system identification number assigned to the claim. Link to open claim by clicking onto the claim ID
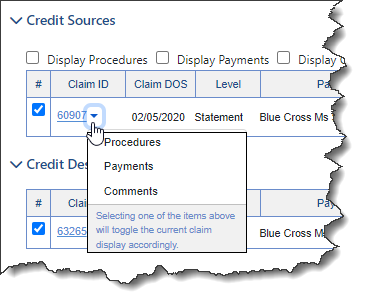
If users don't want to display procedures, payments and comments for all claims in the list, there is an individual claim option by using the dropdown next to the Claim ID
Claim DOS: The service date of the claim.
Level: The level of the claim
Payer: The insurance on the claim associated with the level (primary, secondary, tertiary)
Charges: The sum of charges for this claim.
Payments: The sum of the paid amount for this claim.
Adjustments: The sum of adjustments on this claim.
Balance: The current credit balance of this claim.
- Actions: Icon displaying the source. There can be multiple icons if there are multiple refundees on the claim.
(Tertiary will also be listed as a "T" if there is a tertiary payer on the claim.)
| Resp. Party | Primary | Secondary | Missing | Unaffiliated |
 |  |  |  |
|
| Responsible Party on claim | Primary Insurance on claim | Secondary Insurance on claim | Refund not assigned to payer or responsible party | Refund not assigned to payer/patient assigned to this claim |
Clicking the icon will display available options for switching the refund assignee: 
- Re-assign: Places the refund to the selected assignee
- Unassign Refund: Removes the assignment of an invalid or inaccurate credit from a claim. (Replaces the Refund Maintenance tool)
Credit Destinations
By default, the credit destinations shown will be only claims with patient balances, though that can be changed with a selection box. If a user plans to transfer money between claims, they will choose the appropriate destinations for the money here.
If the 'Auto Distribute when creating a Refund or Transfer' was checked, this screen will show the selected credits distributed across the selected Credit Destinations. If unchecked, the screen will start with no money allocated.
- Checkboxes:
- Display Procedures: Procedures will be displayed for all claims listed
- Display Payments: All payments toward claims will be displayed for all claims listed
- Display Comments: All comments will be displayed for all claims listed
Claim ID: The system identification number assigned to the claim. Link to open claim by clicking onto the claim ID
Claim DOS: The date of service for the claim.
Level: The level listed on the claim (Primary, Secondary, Tertiary, Statement)
Payer: The Payer listed on the claim also associated with the level.
Charges: Total charges billed out on the claim
Payments: All payments applied to claim
Adjustments: Total of all adjustments made on the claim
Balance: The current credit balance of this claim.
Gear Icon
- Company Settings: Select this to be taken to all Company Settings for Credit/Refund(s)
- Refresh: Refreshes screen
Source Actions
- Refund: Select this action to begin processing the credit to the assignee
Destination Actions
- Transfer: Select this action to begin redistribution of the credit
This screen will display claims selected from the Claim Credit Select screen allowing the entry and processing details of the refund(s).
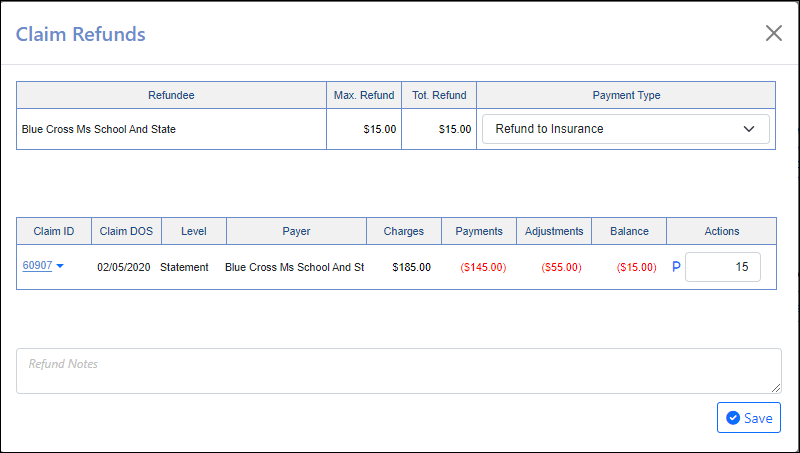
This screen will display claims selected from the Claim Credit Select screen allowing the entry and processing details of the refund(s).
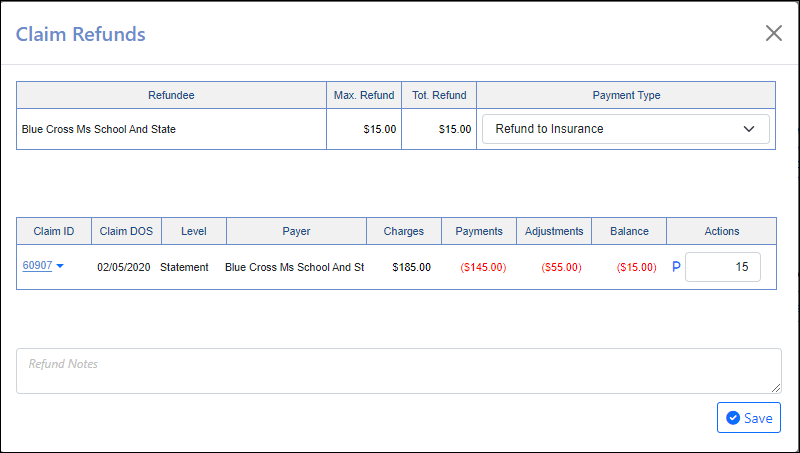
Fields
The Refund Details table, contains the following fields:
Refundee: The responsible party that will be refunded.
Max. Refund: The maximum amount available for refund.
Tot. Refund: The total amount accounted for to be refunded.
Payment Type: The payment type that will be associated with the refund.
Claim ID: The system identification number assigned to the claim. Link to open claim by clicking onto the claim ID
Claim DOS: The date of service for the claim.
Level: The level listed on the claim (Primary, Secondary, Tertiary, Statement)
Payer: The Payer listed on the claim also associated with the level.
Charges: Total charges billed out on the claim
Payments: All payments applied to claim
Adjustments: Total of all adjustments made on the claim
Balance: The current credit balance of this claim.
Actions: Amount that will be refunded with a tooltip explaining where the refund will go
Refund Notes: A note that will be added to this refund once saved.
Save: Saves entries from above.
This screen will display claims selected from the Claim Credit Select screen allowing the entry and processing details of the Transfer(s).

Fields
The Transfer Details table, contains the following fields:
Patient: The patient’s account number and name. This can be double-clicked to open the patient summary.
Current Balance: Balance for claims to date
Available Credit: The patient’s total credit balances before the transfer.
Updated Credit: What the patient’s total credit balances will be if the transfer is processed as entered.
Available Balance: The patient’s total credit balances before the transfer.
Updated Balance: What the patient’s total open balances will be if the transfer is processed as entered.
Payment Method: The payment method that will be associated with the transfer. (Default: Transfer)
Payment Type: The payment type that will be associated with the transfer. (Default: Payment Transfer)
Claim ID: The system identification number assigned to the claim. Link to open claim by clicking onto the claim ID
Claim DOS: The date of service for the claim
Level: The level listed on the claim (Primary, Secondary, Tertiary, Statement)
Payer: The Payer listed on the claim also associated with the level.
Charges: Total charges billed out on the claim
Payments: All payments applied to claim
Adjustments: Total of all adjustments made on the claim
Balance: The current credit balance of this claim.
Actions: Amount that will be transferred with a tooltip explaining where the it will go
Claim ID: The system identification number assigned to the claim. Link to open claim by clicking onto the claim ID
Claim DOS: The date of service for the claim.
Level: The level listed on the claim (Primary, Secondary, Tertiary, Statement)
Charges: Total charges billed out on the claim
Payments: All payments applied to claim
Adjustments: Total of all adjustments made on the claim
Balance: The current credit balance of this claim.
Allocate: Amount to be transferred from Available Credit to this claim
Transfer Notes: A note that will be added to the transfers when they are saved.
Save: Saves entries from above