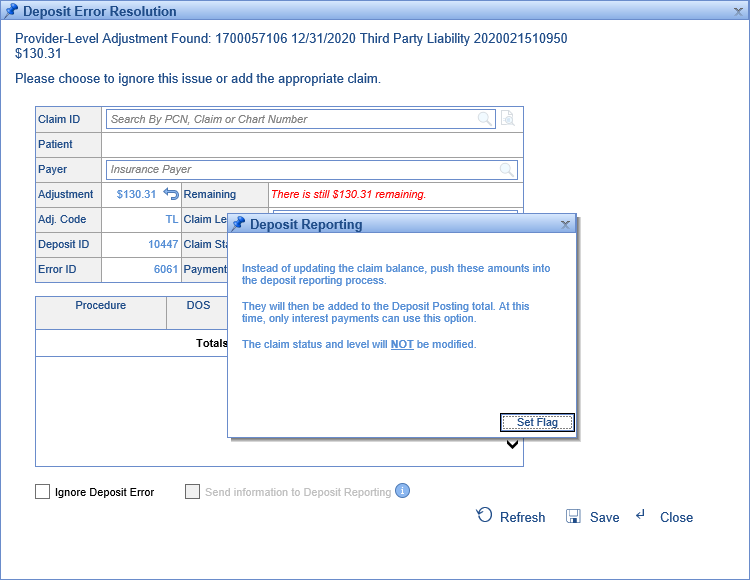
When posting Provider- and Claim-Level Adjustments, users have the option to, instead of posting the money to lines, send it to Deposit Reporting.
If sent to deposit reporting, these amounts aren't posted to claims -- they don't affect claim balances, so they don't need to be adjusted, and they won't show up on statements. They won't appear in the Practice Summary, or Billing Analytics. Instead, they fall outside regular financial reporting, to be reported on and (if necessary) distributed to providers separately.
There are two ways to send ERA Amounts to Deposit Reporting:
- Sending Manually
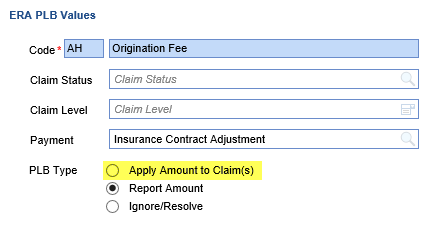
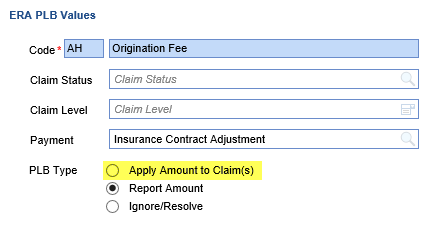
- Set the adjustment code in question to "Apply Amount to Claim(s)."
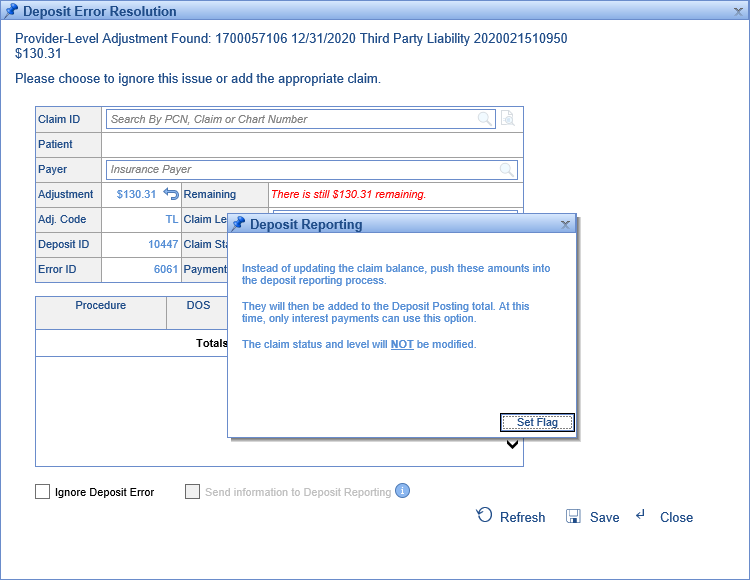
- When posting the adjustment, check the box at the bottom of the screen to "Send information to Deposit Reporting." Sometimes this requires clicking the 'i' to set the flag.
- Set the adjustment code in question to "Apply Amount to Claim(s)."
- Sending Automatically
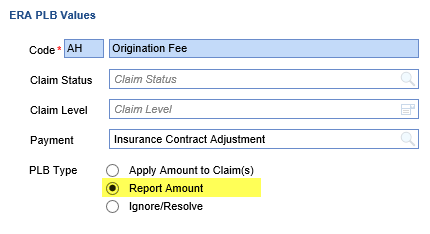
- Set the ERA Amount in question to "Report Amount."
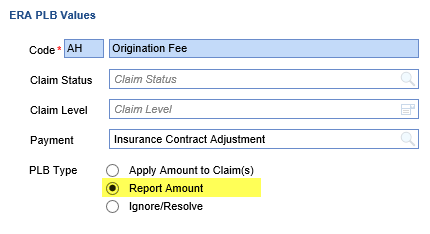
This will cause these errors to auto-resolve, with the associated claim or PLB adjustment code automatically showing up with the designated payment type in Deposit Reporting.
- Set the ERA Amount in question to "Report Amount."
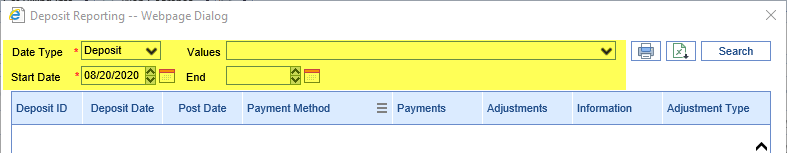
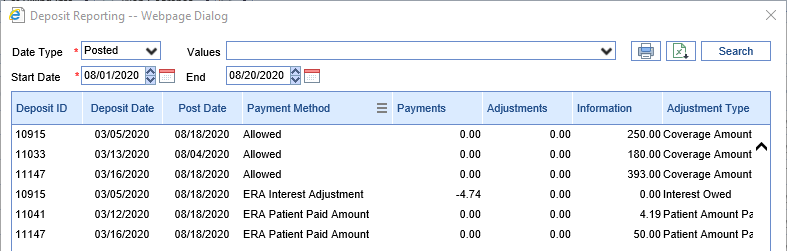
To view Deposit Reporting, click the "More" button on the Deposits screen toolbar, then click "Deposit Reporting":
Parameters:
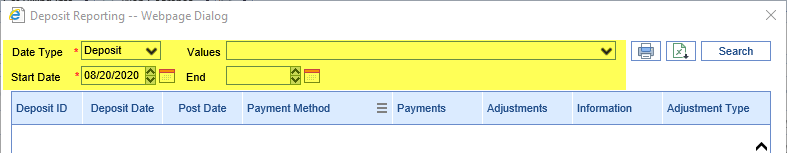
- Date Type: Designates whether the Start Date and End Date selected are the date the deposit was sent to posting or its deposit date.
- Values: A multi-select box allowing users to filter to certain claim/PLB adjustment codes if desired.
- Start Date: The desired start date for the search.
- End Date: The desired end date for the search.
Columns
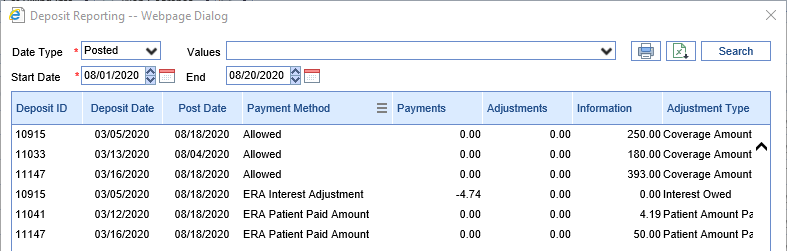
- Deposit ID: The ID of the deposit containing this Claim- or Provider-Level adjustment.
- Deposit Date: The deposit date of the deposit in question.
- Post Date: The date the deposit in question was sent to posting.
- Payment Method: The Payment Type chosen for this adjustment. This is what will be used to decide if the amount is being reported as a payment, an adjustment, or only an informational amount.
- Payments: If the selected payment type's setup has "Affects Payment" checked and "Comment Indicator" unchecked, it will be considered a payment.
- Adjustments: If the selected payment type's setup has "Affects Payment" and "Comment Indicator" both unchecked, it will be considered an adjustment.
- Information: If the selected payment type's setup has the "Comment Indicator" box checked, this ERA Amount will be considered informational.
- Adjustment Type: This is the description of the originating adjustment code, whether it appeared at the claim or provider level.
- Error Type: Denotes whether this amount originated in an error on the Claim or the Deposit.
- Error Description: This is the description of the originating error.
- Payer: This is the payer on the associated deposit.
- Claim ID: If this amount is associated with a claim, this shows the relevant claim ID.
- Claim Provider: If this amount is associated with a claim, this shows the relevant Rendering Provider from the claim.
Additional Report Options

- Print: This option opens a printable PDF of the report.
- Export: This option exports the report to Excel.