Error Level: Claim
Error Message: The claim referenced in the ERA cannot be found.
Actions to Take: User should resolve the error by associating the selected claim from the deposit with a claim that exists in the application. If this claim exists in another system, it may be best to Ignore this error.
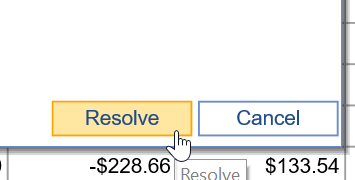
- Click Resolve on the Deposit Claim.
- Choose to ignore or to adjust the procedure payment to match the carrier payment.

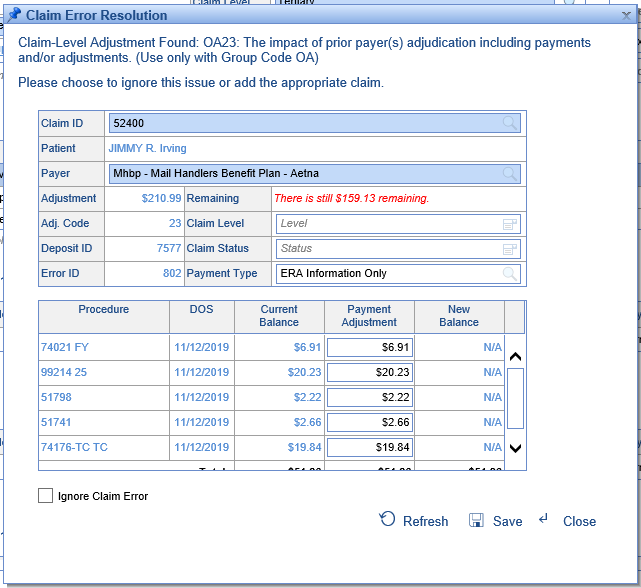
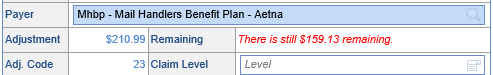
About this Error: When an ERA is received, it's possible for the paid amount the payer included in the line-level information to be reduced by a claim-level adjustment. If this is the case, you'll want to resolve the payer mismatch error to accordingly reduce the payment recorded in the posting.
Error Level: Claim
Error Message: The claim referenced in the ERA cannot be found.
Actions to Take: User should resolve the error by associating the selected claim from the deposit with a claim that exists in the application. If this claim exists in another system, it may be best to Ignore this error.
- Click Resolve on the Deposit Claim.
- Either exclude the claim or search for the claim using the patient name, service date, or claim number.
- Click Resolve
About this Error: When an ERA is received, the 835 ERA file will contain a Patient Control Number (PCN) in field CLP 01. This is a unique value generated by the system that originally submitted the claim. This is how the claim in the ERA is associated to the claim in the application. In some scenarios, the ERA contains claims that were not generated in our application and the association can not be made automatically.
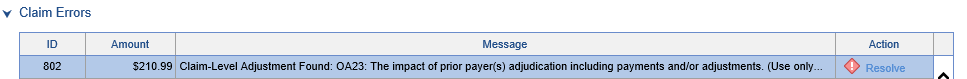
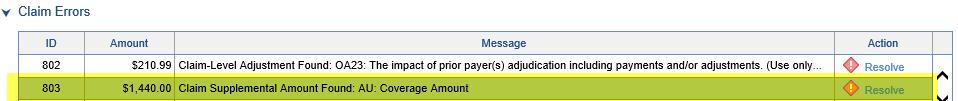
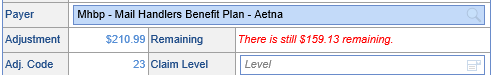
Error Level: Claim
Error Message: At least one claim-level adjustment was found.
Actions to Take: Please choose to ignore this issue or add the appropriate claim.
- Click Resolve
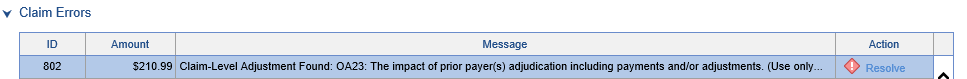
The fields will be populated with information from the claim, and its procedure lines will be displayed. The application will attempt to associate the Adjustment Amount with the correct procedure lines based on the outstanding balance of those procedures.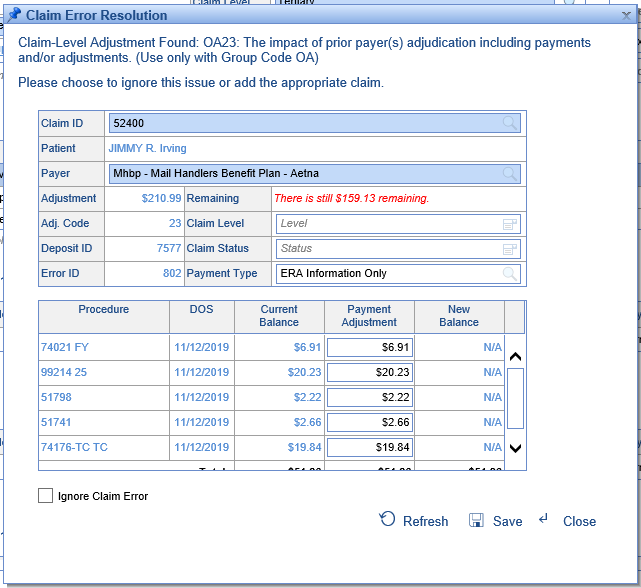
- Make any necessary changes to the posting information that you desire.
NOTE: If you do not allocate the entire adjustment amount, the error will still exist: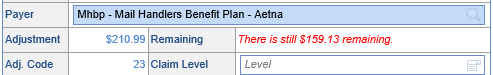
- Click Save.
About this Error: This error occurs because a claim-level adjustment was found, and the system needs additional information to apply the money or ignore it.
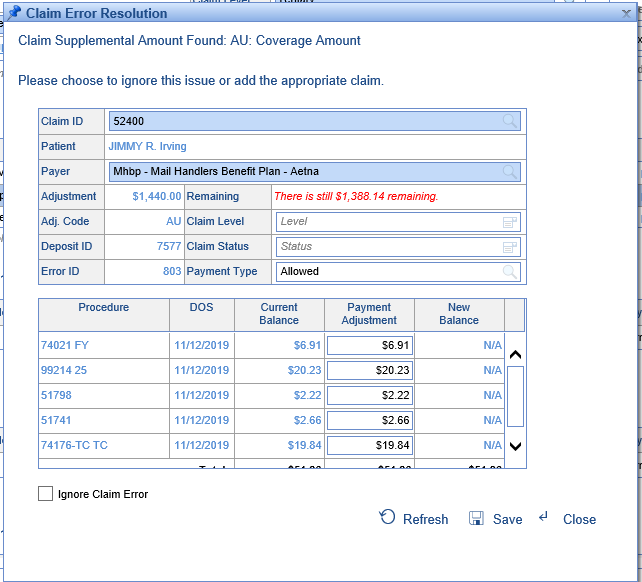
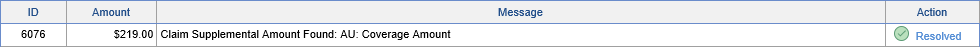
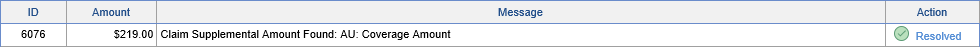
Error Level: Claim
Error Message: At least one claim supplemental amount was found.
Actions to Take: Please choose to ignore this issue or add the appropriate claim.
Note: If you're seeing a Claim Supplemental Amount with the code AU, this likely needs to be ignored, and modified to always be ignored in the setup.
- Click Resolve
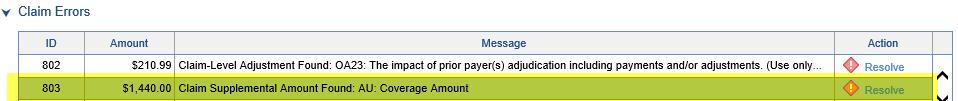
The fields will be populated with information from the claim, and its procedure lines will be displayed. The application will attempt to associate the Adjustment Amount with the correct procedure lines based on the outstanding balance of those procedures.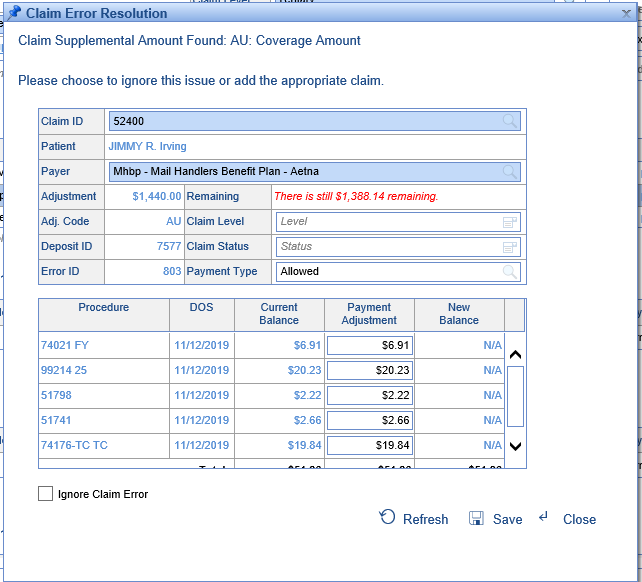
- Make any necessary changes to the posting information that you desire.
NOTE: If you do not allocate the entire adjustment amount, the error will still exist: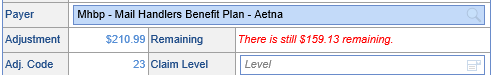
- Click Save.
About this Error: This error occurs because a claim supplemental amount was found, and the system needs additional information to apply the money or ignore it.
Error Level: Claim
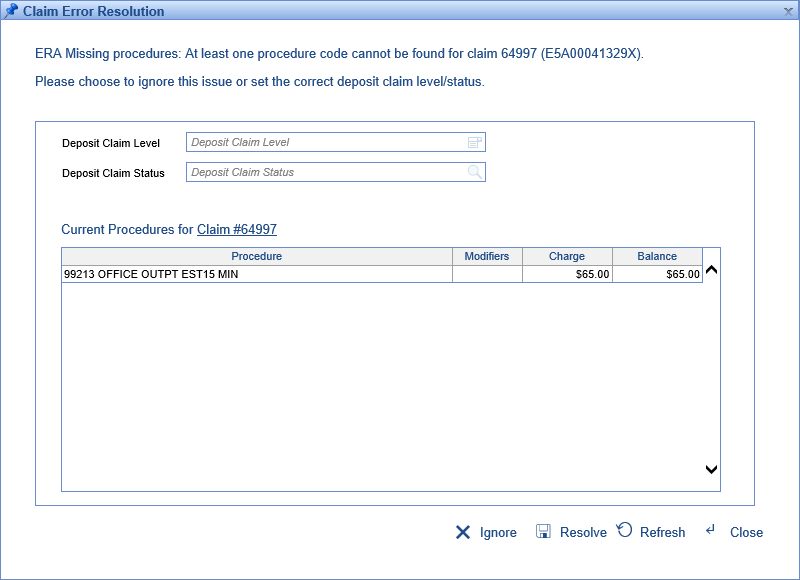
Error Message: At least one procedure code cannot be found for claim [Claim ID].
Actions to Take: Please choose to ignore this issue or set the correct deposit claim level/status.
- Click Resolve.
The resolution screen will show the current procedures for the claim as follows: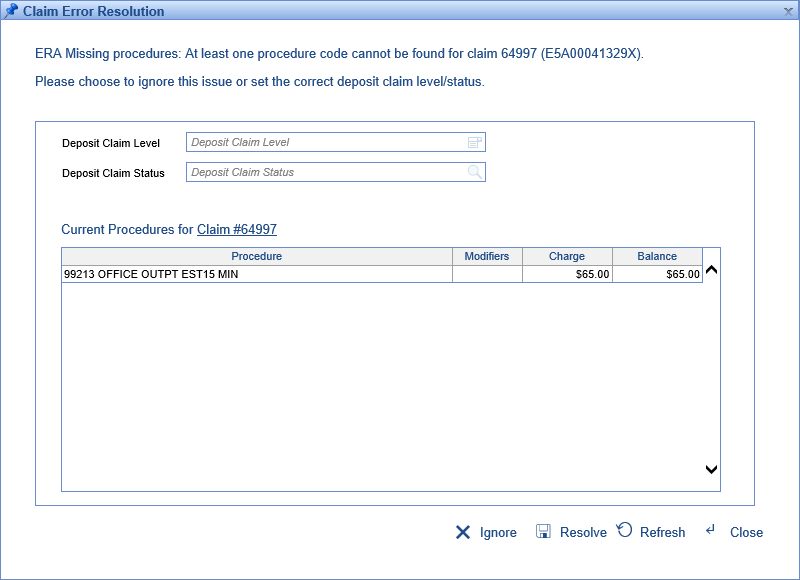
- Compare the procedures on the claim with those on the ERA and make any necessary changes to the deposit claim level/status. Otherwise, choose to "Ignore" this error.
About this Error: Sometimes claims have procedure lines that are not addressed by incoming ERAs. Previously, because there wasn't a denial being posted, the system was allowing these claims to move to the next level/status. Now, the system will throw an error, "ERA Missing Procedures," allowing the user to find these instances and modify the claim level and status accordingly.
Error Level: Claim
Error Message: Invalid Recoup
Actions to Take: User should review the claim/status to make sure they are correct considering that this recoup was posted.
- Click Resolve

- Review the previous payments for the claim in question either by looking at the listed payments or clicking the link for Claim # ______. Upon making the determination on the validity of the recoup, and whether the claim and status have been set correctly, the user can either choose to exclude this deposit claim, set the level/status differently, or ignore this error.

About this Error: Sometimes a payer will send a payment and a recoup for that payment in the same ERA. In those instances, if the recoup was listed before the payment, the system would post the recoup first, then the payment. Because the payment would look like a full payment, the status/level would be set as if the line was paid even though the payment had already been recouped. This could cause the line to progress to the next payer or the patient!
To fix this, we have created a claim error that triggers when a recoup is being posted with no originating payment from the same payer. This will ‘hold’ this posting so that it can occur after the associated payment. The most you'll need to do is double-check the validity of the recoup and that the resulting claim level and status are what you'd want them to be-- if those values look good, you can ignore this error.
Error Level: Claim
Error Message: Unable to determine payer for this claim's payments.
Actions to Take: Please connect the claim to a insurance payer. Note that you may first need to update the claim if it doesn't have the correct payer attached.
About this Error: You may see this error if a payment comes in from a secondary crossover insurance that isn't on the claim -- in this case, you will need to update the claim with the correct secondary, and click "Resolve" on the error to attach this insurance to the posting.
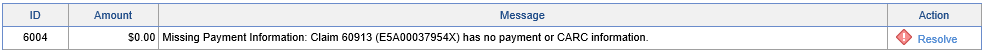
Error Level: Claim
Error Message: Missing Payment Information
Actions to Take: Either ignore or set the correct claim level/status.
- Click Resolve
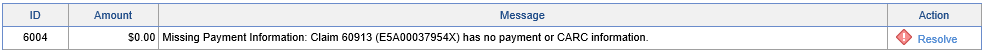
- Make the determination on whether the level and status are as desired. If so, ignore the error -- otherwise, you can set them here and click Resolve.

About this Error: On posting a deposit claim, the system will check to see if on any given line the paid and allowed amounts are $0, no CARC codes have been added, and the Charge amount is greater than $1. If this is the case, it’s likely that the payer has neglected to send some sort of key information. If that's the case, this is an opportunity to set the level and status to prompt a review, or if it's expected, this error can be resolved.
Error Level: Claim
Error Message: Patient payment import contained error(s).
Actions to Take: Please create a new import for the records in question, correcting any data issues.
About this Error: This error can occur if the format is incorrect on the patient payment document you attempted to import. If you fix the errors in your document, you can attempt this import again.
Error Level: Claim
Error Message: <ERA Payer Name> indicated that this claim was <Remit Status>. Based on how this was processed, it appears the insurances are setup incorrectly on the claim. Please fix the insurance assignment for this claim or ignore.
Actions to Take: If you've received this error, you likely want to compare the payer on the deposit claim and the payers listed on the claim, to make sure that both are correct. This error gives you the option then to:
- Ignore the error
- Update the payer for the deposit claim
- Change the payer(s) on the claim
About this Error: In the past, if we assigned a deposit claim to be a payer that was the primary on the claim, but the remit status selected was "Processed as Secondary," the posting would go through as entered. Now the remit status and level of the selected payer will need to match or an error will be thrown, giving you the opportunity for review.
Error Level: Claim
Error Message: Multiple status overrides were found for this procedure.
Actions to Take: Please click "Resolve" next to the error and select the appropriate resulting Claim Status.
About this Error: It's possible for a practice to set up conflicting rules about what status to assign to a claim as the result of the posting process. For instance, if on one code you received a denial due to prior authorization issues, but on another code you received a non-covered denial, it's possible to set these denials to result in two different claim statuses. If this is the case, you will need to manually select the correct status by clicking the "Resolve" button on the error.
Error Level: Claim
Error Message: Multiple level overrides were found for this procedure.
Actions to Take: Please click "Resolve" next to the error and select the appropriate resulting Claim Level.
About this Error: It's possible for a practice to set up conflicting rules about what level to assign to a claim as the result of the posting process. For instance, if one code is paid fully by the primary and would normally go to the secondary, but another code is denied, when posting these the resulting levels would conflict. If this is the case, you will need to manually select the correct level by clicking the "Resolve" button on the error.
Error Level: Claim
Error Message: Patient Responsibility: The patient responsibility amount of <ERA Amount> is different than the remaining balance of <Claim Balance> on the claim.

Actions to Take: If you've received this error, you likely want to compare the "Patient Responsibility" amount found on the human readable ERA with the outstanding balance on the claim. Many times, secondary payers will pay the claim off entirely, but due to some account discrepancies between the Primary Payer and the Secondary Payer, a small balance will remain in our application for this claim. Sometimes this balance just needs written off. Other times, the claim may actually need to go to the patient via a statement. This error gives you the ability to make that decision.
- Ignore the error
- Write off the balance
You can find the 'Patient Responsibility Amount' by opening the EOB linked to the deposit.

About this Error: If the Patient Responsibility on an ERA comes in as $0, the system will now display an error after the posting process if the patient responsibility on the claim in our application is not $0.
This will prevent balances from being sent to patients on statements when they should not be responsible.
Pro Tip: In addition, practices can also use the "Patient Responsibility Claim Status ID" Company Setting to set claims that get this error to a specific status. By moving it to a different status, it will ensure the claim does not get added to a statement batch before the posting team has had a chance to resolve that error.
Error Level: Claim
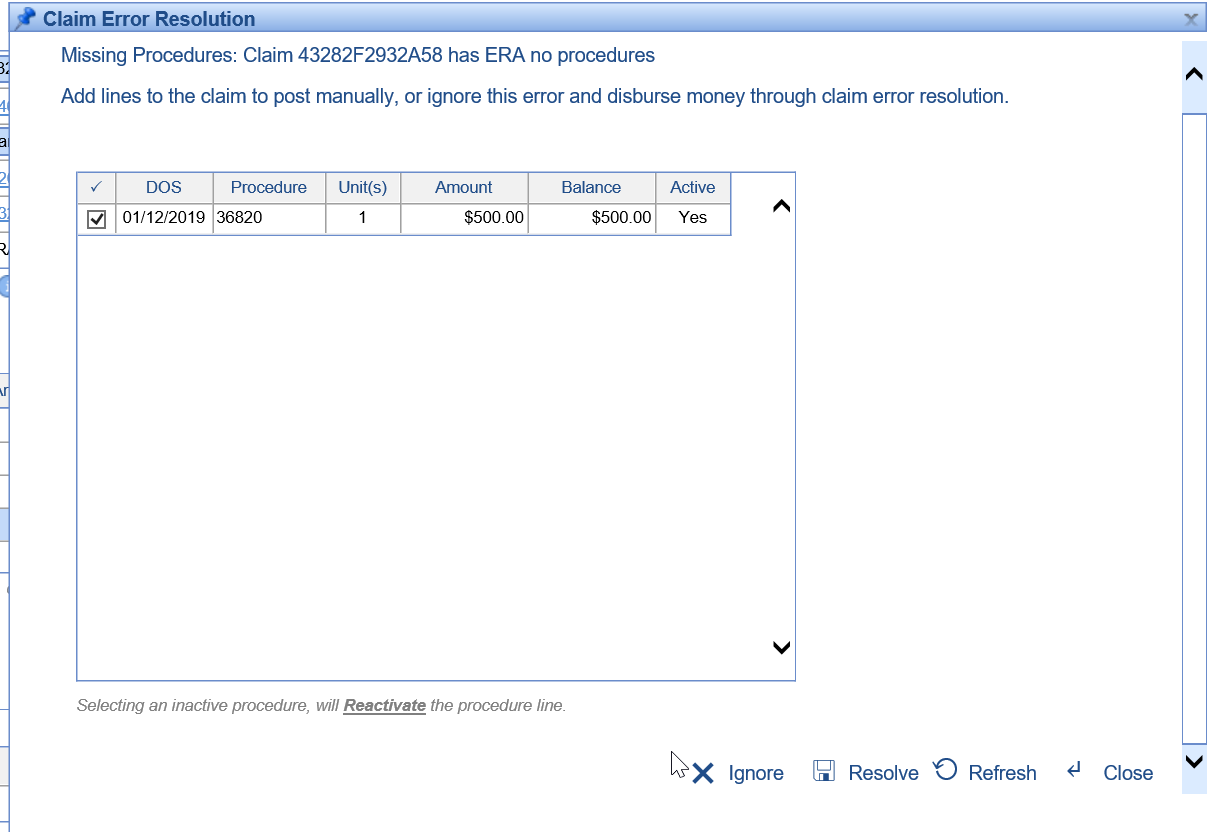
Error Message: Missing Procedures: Claim has no ERA Procedures.

Actions to Take: If you've received this error, it is possible that the ERA was sent without procedure lines. This happen from time to time and is most likely an error that the payer made when generating the ERA file. This is helpful in identifying these scenarios so that the ERA is not posted incorrectly. Use this as an opportunity to review the human readable ERA and add the necessary procedure lines manually when appropriate.
Steps to Resolve
- Click Resolve
- Decide if you would like to manually add the procedure information by pulling in procedures from the claim. The error resolution window will display all procedures that are on the claim in our application.
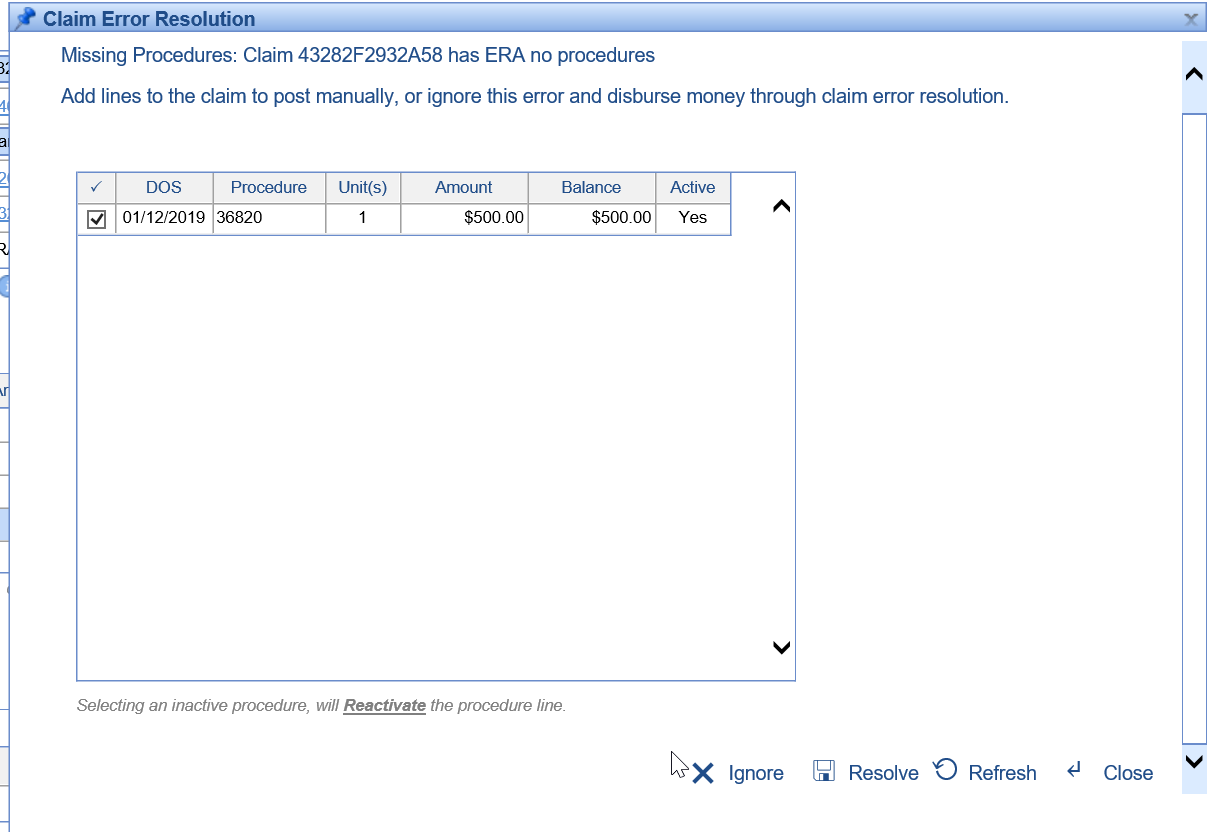
- If the procedure information was not provided, it may be best to Ignore this error and Exclude this Claim from the batch all together.