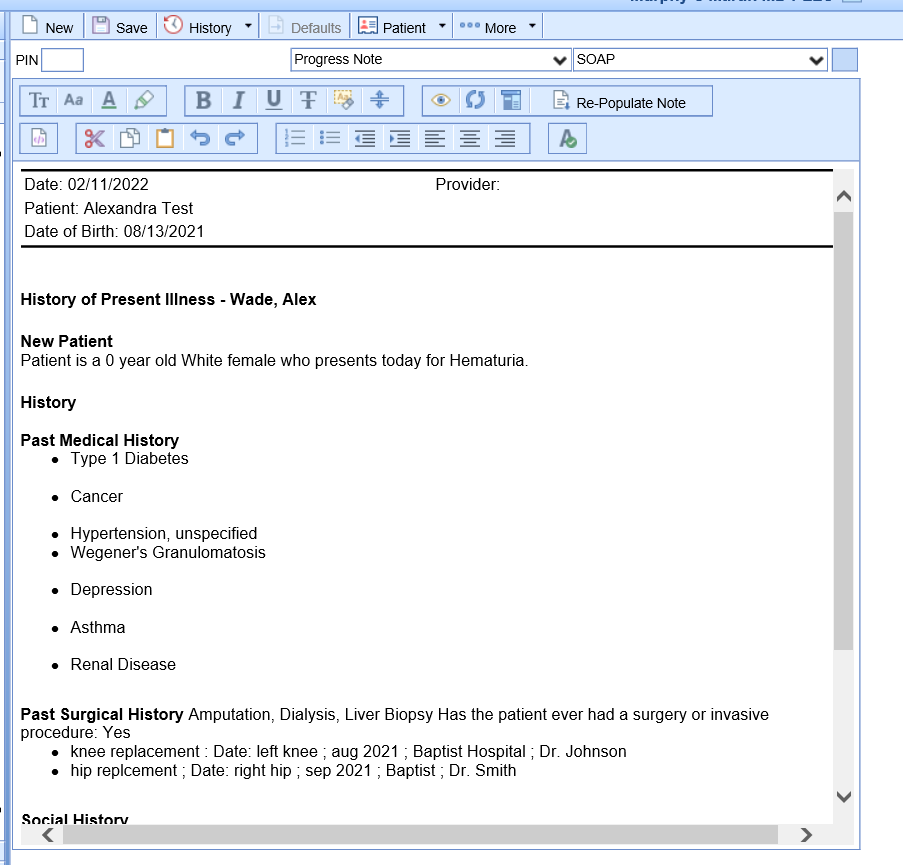
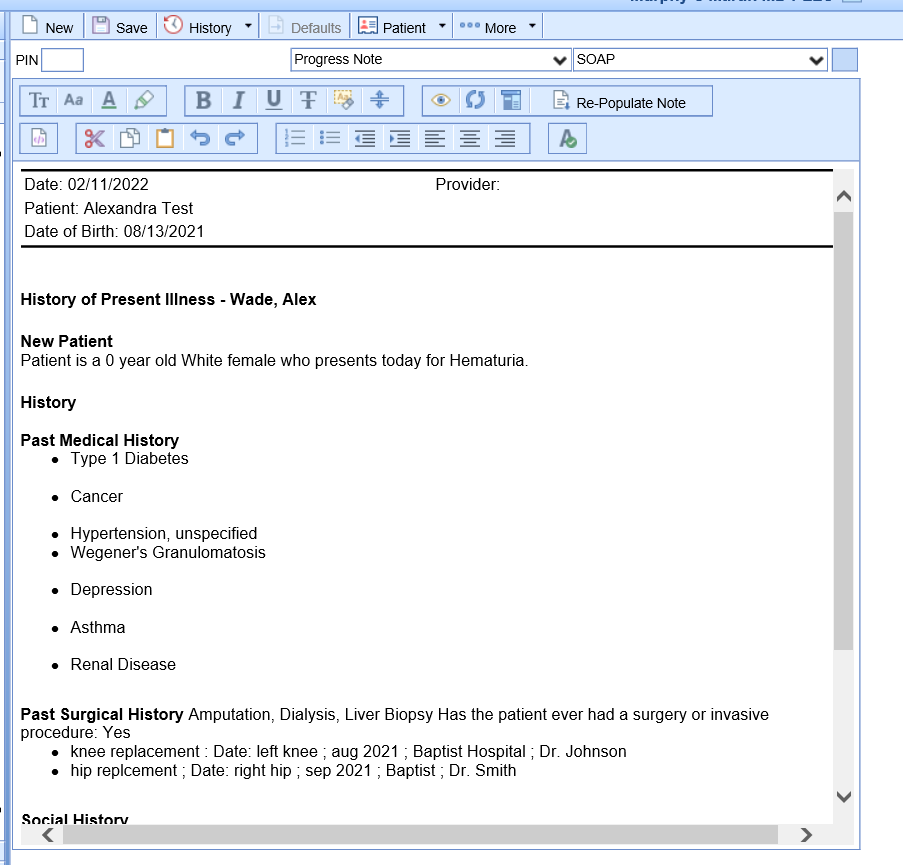
The SOAP Note chart tab is a dynamic chart tab in which data pulls for various chart tabs to create a formal visit note. Users may have various SOAP Note letters to choose from when creating a SOAP Note.
Navigating to the SOAP Note Chart Tab
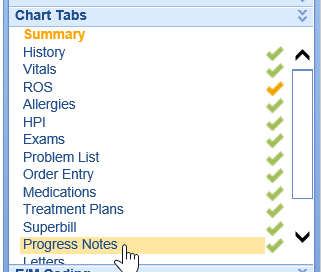
- Begin by documenting all aspects of the visit. (For example, History, Vitals, Allergies, ROS, HPI, Exams, Problem List, Medications, Orders, Treatment Plan, Superbill, etc)
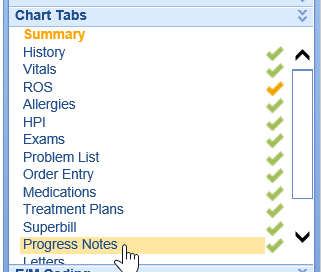
- Navigate to the SOAP Notes chart tab, the system will generate a SOAP Note based on the user's default SOAP Note letter.
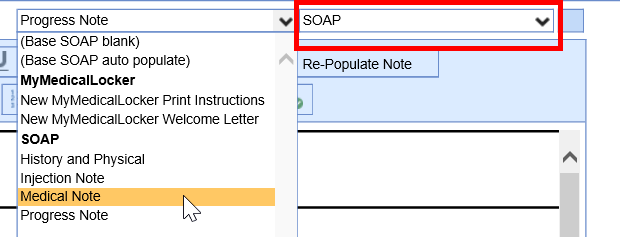
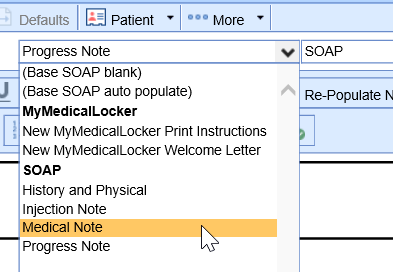
- Users may choose to change the SOAP Note letter by selecting a new template from the first dropdown.
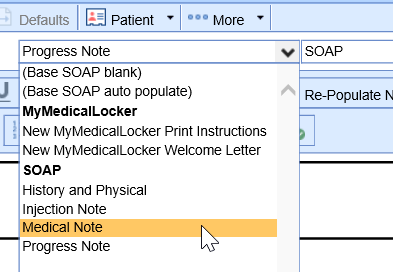 In most cases, the SOAP Note type will generate on it's own based on the SOAP Note letter template settings.
In most cases, the SOAP Note type will generate on it's own based on the SOAP Note letter template settings. 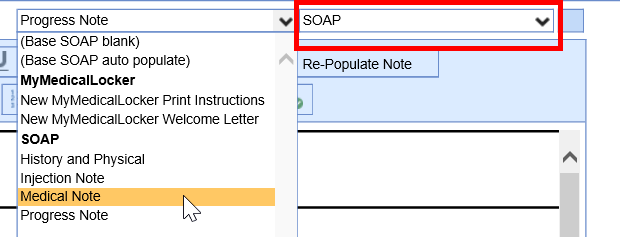
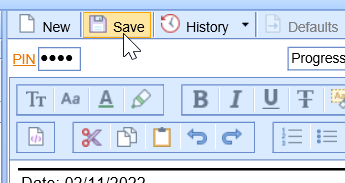
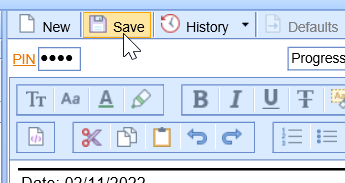
- Once the user has reviewed the note and is ready to sign-off, navigate to the PIN box and enter their unique 4-digit pin. Click Save.
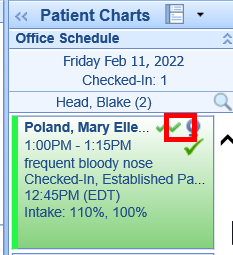
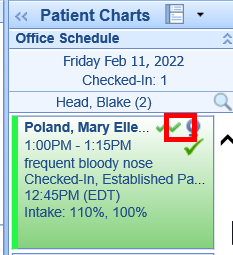
- For scheduled visits, a signed SOAP Note will be indicated using a green check mark on the appointment.
NOTE: Practices may use various terminology when labeling the final office note. (I.E. Progress Note, Visit Note, SOAP Note, etc)
 In most cases, the SOAP Note type will generate on it's own based on the SOAP Note letter template settings.
In most cases, the SOAP Note type will generate on it's own based on the SOAP Note letter template settings.