Medicare Telehealth Frequently Asked Questions (FAQs)
March 17, 2020
- Q: How will recently enacted legislation allow CMS to utilize Medicare telehealth to address the declared Coronavirus (COVID-19) public health emergency?
A: The Coronavirus Preparedness and Response Supplemental Appropriations Act, as signed into law by the President on March 6, 2020, includes a provision allowing the Secretary of the Department of Health and Human Services to waive certain Medicare telehealth payment requirements during the Public Health Emergency (PHE) declared by the Secretary of Health and Human Services January 31, 2020 to allow beneficiaries in all areas of the country to receive telehealth services, including at their home.
- Q: What does this mean? What payment requirements for Medicare telehealth services are affected by the waiver?
A: Under the waiver, limitations on where Medicare patients are eligible for telehealth will be removed during the emergency. In particular, patients outside of rural areas, and patients in their homes will be eligible for telehealth services, effective for services starting March 6, 2020.
- Q: Why wasn’t this done before?
A: Current telehealth law only allows Medicare to pay practitioners for services like routine visits furnished through telehealth under certain circumstances. For example, the beneficiary receiving those services must generally be located in a rural area and in a medical facility. Where the beneficiary receives those services is known as the “eligible originating site.” The beneficiary’s home is generally not an eligible originating site, but under the new 1135 waiver, this will be waived during the emergency. This will now allow telehealth services to be provided in all settings – including at a patient’s home.
- Q: What services can be provided by telehealth under the new emergency declaration?
A: CMS maintains a list of services that are normally furnished in-person that may be furnished via Medicare telehealth. These services are described by HCPCS codes and paid under the Physician Fee Schedule. Under the emergency declaration and waivers, these services may be provided to patients by professionals regardless of patient location. Medicare pays separately for other professional services that are commonly furnished remotely using telecommunications technology without restrictions that apply to Medicare Telehealth. These services, including physician interpretation of diagnostic tests, care management services and virtual check-ins, are normally furnished through communication technology.
- Q: Would physicians and other Qualified Providers be able to furnish Medicare telehealth services to beneficiaries in their homes?
A: Yes. The waiver temporarily eliminates the requirement that the originating site must be a physician’s office or other authorized healthcare facility and allows Medicare to pay for telehealth services when beneficiaries are in their homes or any setting of care.
- Q: Who are the Qualified Providers who are permitted to furnish these telehealth services under the new law?
A: Qualified providers who are permitted to furnish Medicare telehealth services during the Public Health Emergency include physicians and certain non-physician practitioners such as nurse practitioners, physician assistants and certified nurse midwives. Other practitioners, such as certified nurse anesthetists, licensed clinical social workers, clinical psychologists, and registered dietitians or nutrition professionals may also furnish services within their scope of practice and consistent with Medicare benefit rules that apply to all services. This is not changed by the waiver.
- Q: Will CMS enforce an established relationship requirement?
A: No. It is imperative during this public health emergency that patients avoid travel, when possible, to physicians’ offices, clinics, hospitals, or other health care facilities where they could risk their own or others’ exposure to further illness. Accordingly, the Department of Health and Human Services (HHS) is announcing a policy of enforcement discretion for Medicare telehealth services furnished pursuant to the waiver under section 1135(b)(8) of the Act. To the extent the waiver (section 1135(g)(3)) requires that the patient have a prior established relationship with a particular practitioner, HHS will not conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency.
- Q: Is any specialized equipment needed to furnish Medicare telehealth services under the new law?
A: Currently, CMS allows for use of telecommunications technology that have audio and video capabilities that are used for two-way, real-time interactive communication. For example, to the extent that many mobile computing devices have audio and video capabilities that may be used for two-way, real-time interactive communication they qualify as acceptable technology. The new waiver in Section 1135(b) of the Social Security Act explicitly allows the Secretary to authorize use of telephones that have audio and video capabilities for the furnishing of Medicare telehealth services during the COVID-19 PHE. In addition, effective immediately, the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waive penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency. For more information: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergencypreparedness/index.html
- Q: How does a qualified provider bill for telehealth services?
A: Medicare telehealth services are generally billed as if the service had been furnished in-person. For Medicare telehealth services, the claim should reflect the designated Place of Service (POS) code 02-Telehealth, to indicate the billed service was furnished as a professional telehealth service from a distant site.
- Q: How much does Medicare pay for telehealth services?
A: Medicare pays the same amount for telehealth services as it would if the service were furnished in person. For services that have different rates in the office versus the facility (the site of service payment differential), Medicare uses the facility payment rate when services are furnished via telehealth.
- Q: Are there beneficiary out of pocket costs for telehealth services?
A: The use of telehealth does not change the out of pocket costs for beneficiaries with Original Medicare. Beneficiaries are generally liable for their deductible and coinsurance; however, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
- Q: How long does the telehealth waiver last?
A: The telehealth waiver will be effective until the PHE declared by the Secretary of HHS on January 31, 2020 ends.
- Q: Can hospitals, nursing homes, home health agencies or other healthcare facilities bill for telehealth services?
A: Billing for Medicare telehealth services is limited to professionals. (Like other professional services, Critical Access Hospitals can report their telehealth services under CAH Method II). If a beneficiary is in a health care facility (even if the facility is not in a rural area or not in a health professional shortage area) and receives a service via telehealth, the health care facility would only be eligible to bill for the originating site facility fee, which is reported under HCPCS code Q3014. But the professional services can be paid for.
- Q: Can qualified providers let their patients know that Medicare covers telehealth?
A: Yes. Qualified providers should inform their patients that services are available via telehealth.
- Q: Should on-site visits conducted via video or through a window in the clinic suite be reported as telehealth services?
A: Services should only be reported as telehealth services when the individual physician or professional providing the telehealth service is not at the same location as the beneficiary.
- Q: How is this different from virtual check-ins and e-visits?
A: A virtual check-in pays professionals for brief (5-10 min) communications that mitigate the need for an in-person visit, whereas a visit furnished via Medicare telehealth is treated the same as an in-person visit, and can be billed using the code for that service, using place of service 02 to indicate the service was performed via telehealth. An e-visit is when a beneficiary communicates with their doctors through online patient portals.
- Q: Are the telehealth services only limited to services related to patients with COVID-19?
A: No. The statutory provision broadens telehealth flexibility without regard to the diagnosis of the patient. This is a critical point given the importance of social distancing and other strategies recommended to reduce the risk of COVID-19 transmission, since it will prevent vulnerable beneficiaries from unnecessarily entering a health care facility when their needs can be met remotely. For example, a beneficiary could use this to visit with their doctor before receiving another prescription refill. However, Medicare telehealth services, like all Medicare services, must be reasonable and necessary under section 1862(a) of the Act.
- Q: Will CMS require specific modifiers to be applied to the existing codes?
A: CMS is not requiring additional or different modifiers associated with telehealth services furnished under these waivers. However, consistent with current rules, there are three scenarios where modifiers are required on Medicare telehealth claims. In cases when a telehealth service is furnished via asynchronous (store and forward) technology as part of a federal telemedicine demonstration project in Alaska and Hawaii, the GQ modifier is required. When a telehealth service is billed under CAH Method II, the GT modifier is required. Finally, when telehealth service is furnished for purposes of diagnosis and treatment of an acute stroke, the G0 modifier is required.
- Q: What flexibilities are available in the Medicaid program to provide care via telehealth for individuals who are quarantined or self-isolated to limit risk of exposure?
A: States have broad flexibility to cover telehealth through Medicaid. No federal approval is needed for state Medicaid programs to reimburse providers for telehealth services in the same manner or at the same rate that states pay for face-to-face services. A state plan amendment would be necessary to accommodate any revisions to payment methodologies to account for telehealth costs. More information is available here.
Question
What is the difference between Telehealth, Telemedicine, eVisits, and and Virtual Check-Ins?
Answer
| Type of Service | Definition | CPT Codes | Patient Relationship with Provider | Additional Information |
|---|---|---|---|---|
| Telehealth | A visit with a provider that uses telecomunication systems between a provider and a patient (AnywhereCare) | 99201-99215 (Office or other outpatient visits) | New or established patients. | These are to be submitted with the appropriate telehealth modifier (Medicare requires the use of POS 02 - Telehealth). |
| Telemedicine | Patient phone calls. | 99241-99243 | Established patients only. | Not originating from a related E&M service provided within the previous 7 days nor leading to an E&M service or procedure within the next 24 hours or soonest available appointment. *Time based. |
| Virtual Check In | A remote evaluation of recorded video and/or images submitted by an established patient. | G2012, G2010 | Established patients only. | Not originating from a related E&M service provided within the previous 7 days nor leading to an E&M service or procedure within the next 24 hours or soonest available appointment. *Time based. |
| E-Visits | A communication between a patient and their porivder through an online patient portal (i.e. MyMedicalLocker) | 99241-99243 | Established patients only. | Can only be used for a cumulative time during 7 days. |
Telehealth or Telemedicine is a new process for many ChoiceEMR users. Along with providers using this functionality, staff will need to know how to bill for these visits as well.
Q. What codes are eligible to be billed as Telehealth visits?
A. Office/Outpatient Visits, 99201-99215; Behavioral Health/Psychotherapy Visits, 90791-90792, 90832-90838, and 90845-90847 (Full list available at CMS.)
Q. Do I need to set up a special Service Location for Telehealth visits? (Updated 4/9/2020)
A. Medicare and many other payers have decided that telehealth claims should be billed with a provider's usual place of service, such as POS 11 - Office. However, your State Medicaid may still require the location POS 02 - Telehealth. It is good to have a separate Service Location for these claims/payers.
Q. Are any modifiers required with these visit codes? (Updated 4/9/2020)
A. Effective 4/1/2020, Medicare is requesting a -95 modifier, or a -GT modifier for Medicare Advantage plans. Commercial payers may require a -95 modifier, or a -GQ modifier, depending on the payer. State Medicaid plans may have their own requirements, so it is important to check with your local plan.
Q. Do I need to set up special Procedure Codes for Telehealth visits? (Updated 4/9/2020)
A. There are two options available with the Choice platform: 1) Create custom Procedure Codes; 2) Use Fee Grouping to allow your usual codes to function as Telehealth codes. When creating these codes, you may want to include a Default Modifier.
Q. Do I need to set up a special Superbill, or a new blue bar on our existing Superbill?
A. It is not required, but many practices find it easier for their provider to select the appropriate codes under a new blue bar on the Superbill.
Q. Can a Telehealth visit be billed from the Superbill in the EMR?
A. Yes. Once the Service Location and the Procedure Codes are set up, then a provider can easily bill a Telehealth visit from the Superbill.
Additional Reference: Medicare Telemedicine Health Care Provider Fact Sheet - CMS
The AnywhereCare telehealth module runs on Google Chrome specifically. When attempting to run a telehealth visit and being unable to start the visit, the below are common troubleshooting tips.
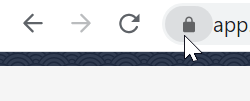
Allow Camera and Microphone Access
- In the Google Chrome URL bar, click the Lock icon.
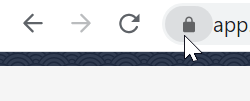
- Set the Microphone, Camera, and Pop-Ups to Allowed.
- Your camera should now be visible in the upper left corner and able to start the Telehealth visit.
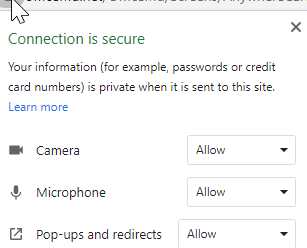
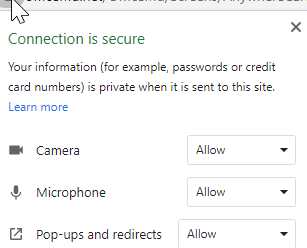
Can't Click "Start Visit" - Chrome Extensions Blocking Access
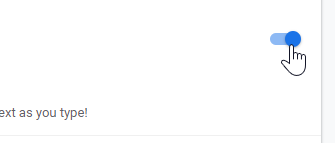
Some Google Chrome extensions, Dragon being a known extension, block access to specific buttons when they are activated.
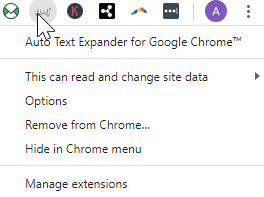
- Right-Click on the Chrome Extension in your browser and select the Manage Extensions option.
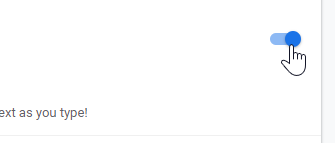
- Inactivate the extension by clicking the slider button.
- Close out of Chrome and re-launch the telehealth visit.
"Unable to Connect"
| Problem/Question My patient is receiving a window that says 'Unable to Connect'. Solution: If the patient receives a window that says, “Unable to Connect”, please instruct the patient to return to the original text/email with the invitation link. By selecting the original link, the session should start automatically. |  |
Logged Out After Telehealth Visit
| Problem/Question Why am I being logged out of my Chrome session of OfficeEMR after an AnywhereCare visit has ended? Solution: This helps to ensure that the provider will remain logged into the database in order to complete any necessary documentation in the patient's chart. |  |
Session Timer Expires During Telehealth
| Problem/Question Why does my session timer log me out of the database during my AnywhereCare visit? Solution: If prompted to Reset the Session Timer from the pop-up, please select the link at the bottom of the pop-up to prevent being logged out of the database and potentially the telehealth session. |  |
"Save My Place in the App"
Problem/Question: My patient has the app already downloaded but is getting this prompt from a telehealth session link instead of opening the session. Solution: When newer OS versions are released, older versions are not supported the same way for Apple and Android devices. |  |
Why does the user see this message: "The following permissions are required to start a telehealth session..."?
AnywhereCare: The following permissions are required to start a visit.
| Problem/Question Why does my patient say that they are getting a message on AnywhereCare that states the following: The following permissions are required to start a telehealth session: Microphone, Camera, Location Services. To turn these permission on: 1. Go to your settings. Select AnywhereCare and allow access to the Location, Microphone & Camera. 2. Close the AnywhereCare app. 3. Click on the link you received in the email/text to start your telehealth session. Solution: This message appears when the user has intentionally or inadvertently selected the 'Do Not Allow' option on their phone when they are prompted.To fix this, the user should follow the below steps in the message. The steps are specific to the device the patient is using. For IOS, be sure the settings screen looks like this:  |  |
Patient Received 2 Messages
Problem/Question Solution: |  |